UCLA researchers using a model of airway tissue created from human stem cells have pinpointed how smoking cigarettes causes more severe infection by SARS-CoV-2, the virus that causes COVID-19, in the airways of the lungs.
The study, led by scientists at the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA and published in Cell Stem Cell, will help researchers better understand COVID-19 risks for smokers and could inform the development of new therapeutic strategies to help reduce smokers' chances of developing severe disease.
Cigarette smoking is one of the most common causes of lung diseases, including lung cancer and chronic obstructive pulmonary disease, and most demographic studies of COVID-19 patients have indicated that current smokers are at increased risk of severe infection and death. But the reasons why have not been entirely clear.
To help understand how smoking affects SARS-CoV-2 infection on a cellular and molecular level, Dr. Brigitte Gomperts partnered with co-senior authors Vaithilingaraja Arumugaswami, an associate professor of molecular and medical pharmacology, and Kathrin Plath, a professor of biological chemistry, to recreate what happens when the airways of a current smoker are infected with SARS-CoV-2.
The team utilized a platform known as an air–liquid interface culture, which is grown from human airway stem cells and closely replicates how the airways behave and function in humans. The airways, which carry air breathed in from the nose and mouth to the lungs, are the body's first line of defense against airborne pathogens like viruses, bacteria and smoke.
"Our model replicates the upper part of the airways, which is the first place the virus hits," said Gomperts, a professor pulmonary medicine and member of the UCLA Jonsson Comprehensive Cancer Center. "This is the part that produces mucus to trap viruses, bacteria and toxins and contains cells with finger-like projections that beat that mucus up and out of the body."
The air–liquid interface cultures used in the study were grown from airway stem cells taken from the lungs of five young, healthy, nonsmoking tissue donors. To replicate the effects of smoking, the researchers exposed these airway cultures to cigarette smoke for three minutes per day over four days.
"This type of model has been used to study lung diseases for over a decade and has been shown to mimic the changes in the airway that you would see in a person who currently smokes," said Gomperts, who is also vice chair of research in pediatric hematology-oncology at the UCLA Children's Discovery and Innovation Institute.
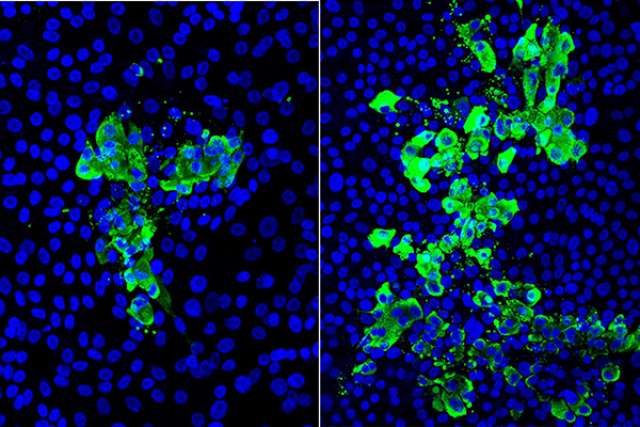
Next, the group infected the cultures exposed to cigarette smoke — along with identical cultures that had not been exposed — with live SARS-CoV-2 virus, and the two groups were compared. In the models exposed to smoke, the researchers saw between two and three times more infected cells.
Digging further, the researchers determined that smoking resulted in more severe SARS-CoV-2 infection, at least in part, by blocking the activity of immune system messenger proteins called interferons. Interferons play a critical role in the body's early immune response by triggering infected cells to produce proteins to attack the virus, summoning additional support from the immune system, and alerting uninfected cells to prepare to fight the virus. Cigarette smoke is known to reduce the interferon response in the airways.
"If you think of the airways like the high walls that protect a castle, smoking cigarettes is like creating holes in these walls," Gomperts said. "Smoking reduces the natural defenses and that allows the virus to set in."
Co-first authors of the study are Arunima Purkayastha, Chandani Sen, Gustavo Garcia Jr. and Justin Langerman, all of UCLA.
This work was supported by the National Institutes of Health, the UCLA Medical Scientist Training Program, a UCLA David Geffen School of Medicine–Broad Stem Cell Research Center COVID-19 Research Award, the California Institute for Regenerative Medicine, the UCLA Clinical and Translational Science Institute (supported by National Institutes of Health's National Center for Advancing Translational Sciences), the Tobacco-Related Disease Research Program, and the Ablon Scholars Program at the UCLA Jonsson Comprehensive Cancer Center and UCLA Broad Stem Cell Research Center.