A new report describes a promising approach to study neurofibromatosis type 1 (NF1), a genetic condition with limited treatment options. The condition causes a number of different cancerous and non-cancerous tumors to form throughout the body. Among these tumors are cutaneous neurofibromas, benign tumors that grow from nerve terminals in the skin.
Current treatment to reduce tumor growth in patients is limited to surgery, which can lead to scarring, re-growth of the tumor and may not be feasible at all when these benign tumors number in the hundreds, or even thousands.
“While benign tumors may not metastasize or spread to other parts of the body, they can still cause substantial health issues, particularly when present in large numbers,” said , an assistant professor in the department of Orthopaedic Surgery at the and member of the . “Given the paucity of options yet severe comorbidities, there is a need to identify new therapeutic avenues to reduce tumor growth in patients.”
The lack of therapies is partly due to the fact that cutaneous neurofibromas are composed of many different cell types and abundant extracellular proteins, making it difficult to model them in the lab to study. To meet these challenges, Soragni and her team has developed a high throughput organoid screening platform to rapidly establish and screen 3D tumor organoids for cutaneous neurofibromas to find drugs that slow tumor growth, supported by a 2018 grant from the .
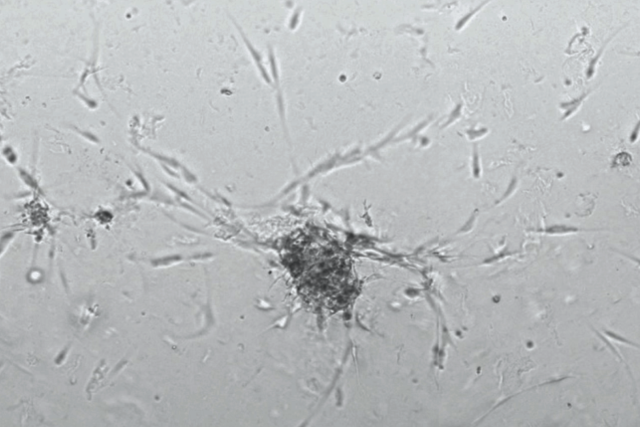
The screening method, described in the journal , uses patients’ own tumor cells, collected during surgery, to create miniature patient-derived tumor organoids. The organoids mimic the characteristics of the tumor they originated from.
By optimizing growth conditions, the team was able to establish patient-derived cutaneous neurofibroma organoids from several patients with NF1, and to show how cutaneous neurofibroma organoids recapitulate the critical features of parental tumors. They also implemented their mini-ring high throughput screening platform to find drugs slowing organoid growth.
Now, thanks to grants from the Gilbert Family Foundation and the Neurofibromatosis Therapeutic Acceleration Program, totaling over $1.6 million combined, the team will use these organoid models to find potential treatments by testing FDA approved drugs to identify the most effective regimen.
The first grant from the Neurofibromatosis Therapeutic Acceleration Program continues the close collaboration with Dr. Sara Gosline, computational biologist at Pacific Northwest National Laboratory. This grant will support the unique effort to develop cutaneous neurofibroma organoid models to pinpoint existing drugs with the potential to treat these tumors and develop biomarkers that indicate whether the patient will respond to that treatment.
Funding from the will support a collaborative effort with Dr. Gosline as well as Dr. Gregory Way at the University of Colorado focused on developing a new type of assay for NF1 organoids called cell painting, which involves tagging different cell components to better understand drug treatment response. This imaging method incorporates machine learning to analyze features of the tumors that may not be apparent to the naked eye. The data will enable the multidisciplinary research team to better investigate how patients may respond to treatments at the cellular level, allowing them to identify lead molecules for further clinical trials.
“Organoid technology represents an enormous opportunity to develop more effective, personalized treatments for NF patients,” said Laura Grannemann, executive director of the Gilbert Family Foundation. “We are very proud to support Dr. Soragni together with Dr. Gosline and Dr. Way in their innovative research and to accelerate cures for NF together.”
Findings from these projects will eventually support translational research efforts at the Nick Gilbert Neurofibromatosis Research Institute (NGNRI), a first-of-its-kind, brick-and-mortar institution devoted to researching NF. The facility, named after the late son of Detroit-area philanthropists Dan and Jennifer Gilbert, is currently under construction in Detroit and will be operational by 2027.
“Because NF1 is a highly complex syndrome with many different manifestations, these grants will help develop therapies for different types of tumors, from benign ones to malignant sarcomas,” said Soragni. “We plan to harness the expertise of our multidisciplinary team with experience in NF1 organoid model development, drug screening, data integration and machine learning. Building directly on our most recent work, we will develop new assays that allow us to couple drug screening with the ability to understand how individual cells respond to the treatment. The end goal is to identify novel drug candidates to treat the diverse tumors affecting NF1 patients.”
Article: A platform for rapid patient-derived cutaneous neurofibroma organoid establishment and screening. Nguyen et al., 2024, Cell Reports Methods 4, 100772. May 20, 2024. DOI: