In an effort to combat one of the most lethal forms of pediatric brain cancer, researchers at the are launching a first-of-its-kind clinical trial to evaluate the safety and effectiveness of a cancer vaccine targeting H3 G34-mutant diffuse hemispheric glioma, a highly aggressive brain tumor that is typically found in adolescents and young adults.
This type of brain tumor is primarily characterized by a particular mutation of the H3-3A gene, which encodes an important regulatory component on histone H3. This mutation leads to significant disruptions in RNA processing, with wide-ranging influences on cancer behavior and response to treatment. The vaccine, developed at UCLA, is designed to target these genetic mutations in these tumors.
One of just a few centers in the United States developing advanced immunotherapies for brain cancer, UCLA Health is the only center investigating immunotherapy for this particular type of glioma.
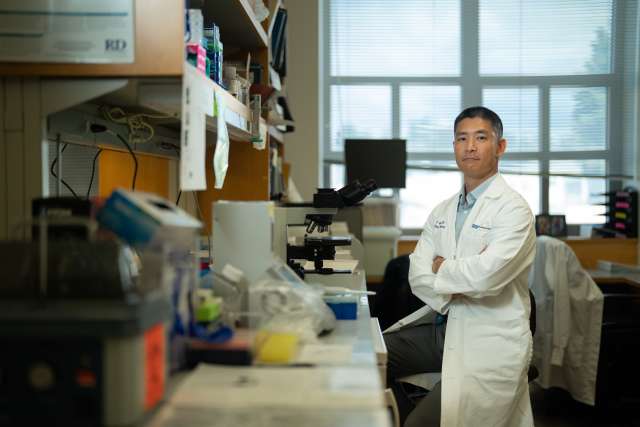
“Despite aggressive treatments, this type of brain tumor evades current therapies with shocking efficiency,” said , director of the and the principal investigator of the trial. “These cancers show a host of escape pathways, allowing small populations of cells to survive initial treatment and to adapt. The data from our pre-clinical studies makes us hopeful that an active, targeted cancer vaccine will be able to adapt with the tumor, in order to eliminate cancer cells more effectively.”
Manufacturing the vaccine
The vaccine works by arming a patient’s dendritic cells, the most efficient activator of the body’s immune system, to target products of the altered RNA regulation that defines this cancer type. Once activated against these targets, the patient’s dendritic cells are then injected back into the patient.
Dendritic cell vaccination in treating some other forms of cancer, including glioblastoma, adding years of life for a subset of patients with a disease that often only has a lifespan of months.
will begin with patients over 18 years old, and will then expand to include patients as young as 5 years old, who have a confirmed diagnosis of H3 G34-mutant diffuse hemispheric glioma. The clinical trial aims to improve survival rates and provide new insights into how the immune system responds to primary brain cancers, and understand whether these targets engender a lasting anti-tumor immune response.
– one of the first university-owned facilities of its kind in the U.S. – will be manufacturing this new dendritic cell vaccine.
The facility’s team of experts, which is led by and Dr. Sujna Raval-Fernandes, provide the skill and resources needed to manufacture the vaccine for a much larger number of patients that meet FDA good manufacturing practice standards.
“Our job is to help accelerate the development of novel cures for a host of illnesses and conditions, including cancer,” said Ward, medical director of the UCLA Human Gene and Cell Facility and associate clinical professor of pathology and laboratory medicine at the David Geffen School of Medicine. “We do this by providing a highly regulated environment to ensure the identity, strength, quality and purity of drug and cell products.”
Laying the groundwork for the clinical trial
The laboratory research leading to this trial has been in development by Wang for several years. In bringing this work to the clinical trial stage, he has worked in collaboration with , chair of neurosurgery at UCLA Health, and , professor in the departments of neurosurgery and molecular and medical pharmacology at the David Geffen School of Medicine at UCLA, who are known for their pioneering work in immunotherapy.
“The development of effective cancer immunotherapies requires a deep understanding of the tumor antigens targeted by the immune system,” said Prins. “And we found that the histone H3 G34R mutation significantly alters mRNA regulation, inducing a conserved set of mRNA splicing changes that result in neoantigens potentially targetable by T lymphocytes.”
Such dysregulation is known to produce immunogenic targets in various cancer types, making it an attractive target for the dendritic cell vaccination.
The UCLA team, in conjunction with professor Yi Xing from the Children’s Hospital of Philadelphia, developed a computational tool named (Isoform peptides from RNA splicing for Immunotherapy target Screening) that predicts products of altered RNA regulation likely to trigger an immune response. Using this tool, the team has identified several neoantigen targets stemming from dysregulated RNA processing, which have proven to be effective targets in laboratory experiments.
“This clinical trial represents a novel and potentially transformative approach to treating high-grade gliomas in children and young adults,” said Liau. “We are optimistic that this research could lead to more advanced studies and eventually a new standard of care for this challenging subtype of brain cancer.”
This line of research is funded in part by grants from the Department of Defense, the National Institutes of Health and by the generous support of donors supporting the UCLA Pediatric Brain Tumor Program.
Take the Next Step
If you think you might be eligible to enroll, or would like to support the development of research like this study, please contact Sichen Li at .