FINDINGS
A UCLA-led team has developed a machine-learning model that can predict with a high degree of accuracy the short-term survival of dialysis patients on Continuous Renal Replacement Therapy (CRRT).
BACKGROUND
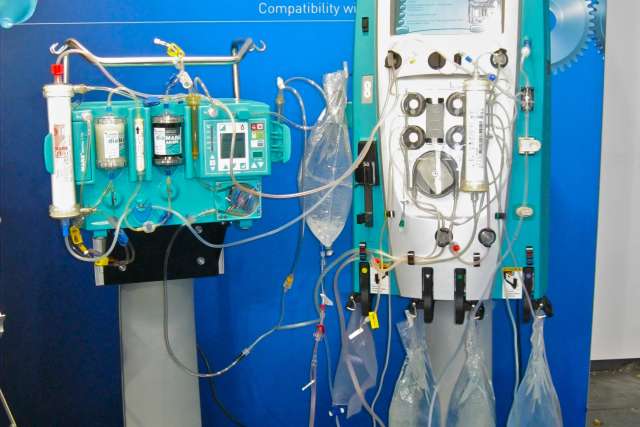
CRRT is a therapy used for very sick hospitalized patients whose health status makes them ineligible for regular hemodialysis. It is a gentler therapy that provides continuous treatment over a prolonged period. About half of adults placed on CRRT, however, do not survive, rendering the treatment futile for both patients and their families.
METHOD
To help doctors decide whether a patient should start CRRT, the researchers developed a machine-learning model that uses data from thousands of patients' electronic health records to predict their chances of surviving the therapy.
IMPACT
The findings provide a data-driven tool to assist in clinical decision-making. This tool incorporates advanced machine-learning techniques to analyze a large and complex set of patient data, which was previously challenging for doctors to do. The study demonstrates how integrating machine-learning models into healthcare can improve treatment outcomes and resource management.
COMMENT
“CRRT is often used as a last resort, but many patients do not survive it, leading to wasted resources and false hope for families,” said Dr. Ira Kurtz, chief of the UCLA Division of Nephrology and the study’s senior author. “By making it possible to predict which patients will benefit, the model aims to improve patient outcomes and resource use, by serving as a basis for testing its utility in future clinical trials. Like all machine learning models, it needs to be tested in the real world to determine whether it is equally as accurate in its predictions in patients that it wasn’t trained on.”
AUTHORS
Additional authors are Davina Zamanzadeh, Jeffrey Feng, Panayiotis Petousis, Arvind Vepa, Majid Sarrafzadeh, and Alex Bui of UCLA, and S. Ananth Karumanchi of Cedars Sinai Medical Center in Los Angeles.
JOURNAL
The study is in the peer-reviewed journal Nature Communications.
FUNDING
This work was supported in part by funds by the Kidney, Urologic, and Hematologic-Advanced Research Training Program (NIH NIDDK U2C DK129496), the Medical Imaging Informatics Training Grant (NIH NIBIB T32 EB016640), the UCLA CTSI grant (NIH UL1 TR001881), the Smidt Family Foundation, the Factor Family Foundation, the Davita Allen Nissenson Research Fund, the Ralph Block Family Fund, and the Kleeman Family Fund.