Key takeaways
- Immunotherapy has been effective in treating certain types of cancer, including those that spread into the brain. But it has little effect in fighting glioblastoma, an aggressive cancer that originates in the brain.
- UCLA-led research revealed that immune checkpoint blockade, a type of immunotherapy, triggers a process that fights tumors more effectively in cancers that spread to the brain than it does in glioblastoma.
- The finding could help scientists develop strategies for more effective immunotherapy for treating brain cancers that originate in the brain, like glioblastoma.
A study led by researchers at the UCLA Jonsson Comprehensive Cancer Center sheds new light on why tumors that have spread to the brain from other parts of the body respond to immunotherapy while glioblastoma, an aggressive cancer that originates in the brain, does not.
In people with tumors that originated in other parts of the body but spread to the brain, treatment with a type of immunotherapy called immune checkpoint blockade appears to elicit a significant increase in both active and exhausted T cells — signs that the T cells have been triggered to fight the cancer. The reason the same thing doesn't occur in people with glioblastoma is that anti-tumor immune responses are best initiated in draining lymph nodes outside of the brain, and that process does not occur very effectively in glioblastoma cases.
To date, immunotherapy has not been effective in treating glioblastoma, but it has been shown to slow or even eradicate other types of cancer, such as melanoma, which frequently metastasizes to the brain.
The new research, published in the Journal of Clinical Investigation, could help improve the effectiveness of immunotherapy for people with brain tumors and it could suggest new paths in the effort to help develop more effective therapies.

“If we’re going to try to develop new therapies for solid tumors, like glioblastoma, which are not typically responsive, we need to understand the tumor types that are responsive, and learn the mechanisms by which that happens,” said the study’s senior author, Robert Prins, a professor of molecular and medical pharmacology and of neurosurgery at the David Geffen School of Medicine at UCLA.
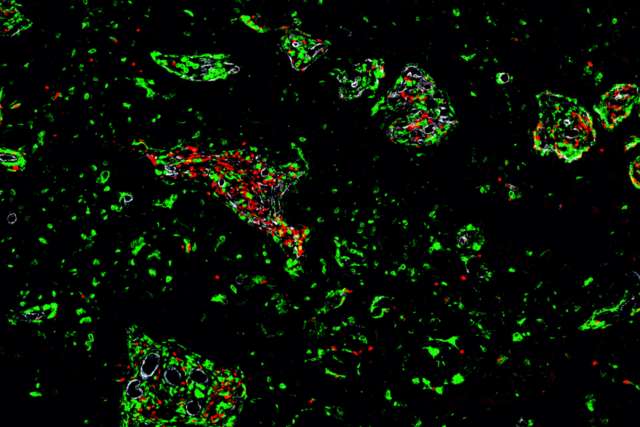
The researchers studied the immune cells obtained from nine people with metastatic brain tumors who had been treated with immune checkpoint blockade — which works by harnessing the body’s immune system to destroy cancer cells — and compared their observations with immune cells taken from 19 patients with brain metastases that not been treated with immunotherapy.
They used a technique called single-cell RNA sequencing from 10x Genomics to examine the genetic material in both sets of samples, and then compared the data to previously published analyses of 25 recurrent glioblastoma tumors to better understand the effect the immunotherapy had on T cells.
“We really were trying to figure out which immune cells are changing in the more responsive tumors in order to better explain the higher response rate to the treatment,” said the study’s co-first author, Lu Sun, a project scientist in the Geffen School of Medicine’s neurosurgery department. “No study has comprehensively examined the differential effect of immune checkpoint blockade treatment on these two types of brain tumors before.”
In the tumors that had spread to the brain, the researchers saw that the T cells had specific characteristics associated with fighting tumors entering the brain, most likely due to a more effective priming step that occurs outside of the brain.
Before traveling to the brain, T cells are first activated in the lymph nodes. During this process, a type of immune cells called dendritic cells share information about the tumor to T cells so they can better attack the tumor. This priming process, however, doesn't work very effectively when doctors attempt to use immune checkpoint blockade for treating glioblastoma.
The researchers also found that a specific subgroup of those exhausted T cells was associated with longer overall survival in people whose cancer had metastasized to the brain.
“We found quite a significant difference between the two types of brain tumors and how they respond to immunotherapies,” said study author Dr. Won Kim, surgical director of UCLA Health’s brain metastasis program and a member of the Jonsson Cancer Center. “There was a tremendous number of T cell lymphocytes that were found within brain metastases following immunotherapy, and while the number of T cell lymphocytes also increased in glioblastoma patients, it wasn’t anywhere near the same extent.”
Prins, who is also a researcher at the Jonsson Cancer Center, said that finding “suggests that enhancing the activation and presentation of T cells by dendritic cells could be a potential treatment strategy.”
In future studies, the researchers plan to analyze data from a larger, more uniform group of people who were diagnosed with melanoma that had spread to the brain.
The study’s other co-first author is Jenny Kienzler, who was a UCLA fellow in neurosurgery when the research was conducted. Other UCLA authors are Jeremy Reynoso, Alexander Lee, Eileen Shiuan, Shanpeng Li, Jiyoon Kim, Lizhong Ding, Amber Monteleone, Geoffrey Owens, Dr. Richard Everson, David Nathanson, Dr. Timothy Cloughesy, Gang Li, Dr. Linda Liau and Willy Hugo.
The research was supported by grants from the National Institutes of Health Specialized Programs of Research Excellence in Brain Cancer, National Cancer Institute, National Institutes of Health National Center for Advancing Translational Science, Parker Institute for Cancer Immunotherapy, Brain Tumor Funder’s Collaborative and Cancer Research Institute.