FINDINGS
A study led by researchers at the UCLA Jonsson Comprehensive Cancer Center suggests that IL-21, a soluble molecule involved in activating the immune system, can be a potential therapeutic target to help reduce endocrine autoimmune side effects caused by checkpoint inhibitor cancer therapy.
The investigators found that a specific group of CD8+ immune cells with strong killing activity, called CXCR6+ IFN-g+ cytotoxic CD8+ T cells, play a central role in this autoimmune attack. They also found the activity of these CD8+ cells were controlled by IL-21 and blocking IL-21 prevented thyroid autoimmunity.
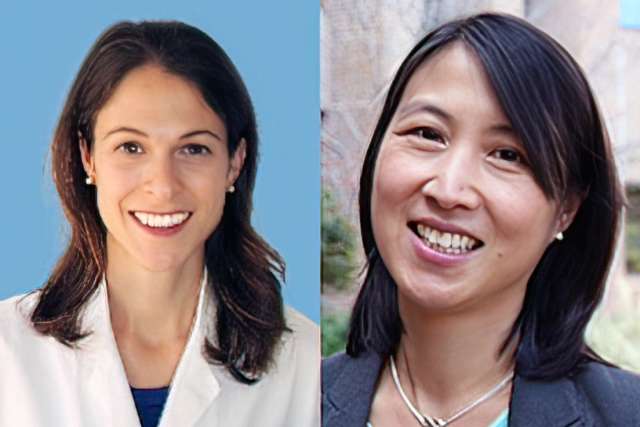
“Our study is the first to provide an in-depth look at the cause of checkpoint inhibitor associated thyroid autoimmunity in humans and highlights a potential pathway for preventing this treatment-related autoimmune toxicity,” said Dr. Melissa Lechner, an assistant professor of Medicine in the division of Endocrinology, Diabetes, and Metabolism at the David Geffen School of Medicine at UCLA and first author of the study.
BACKGROUND
Checkpoint inhibitors are a type of cancer therapy that harnesses the power of the immune system to fight cancer cells and have shown to have remarkable success in treating multiple types of advanced cancers. While this type of therapy has changed the face of cancer treatment, with increased immune activation can come unwanted autoimmune attack on healthy tissues. Such immune related adverse events occur in up to 60% of patients treated with the therapy and can contribute to treatment interruption, hospitalizations, and even premature death.
The cause of these autoimmune toxicities remains largely unknown. Presently there are no effective treatments to prevent or reverse these endocrine immune adverse effects during cancer immunotherapy, which almost universally result in permanent organ damage and lifelong requirement for hormone replacement therapy.
METHOD
To investigate the cause of autoimmune toxicities that occur during checkpoint inhibitor cancer therapy, the team used single cell RNA sequencing of thyroid specimens from patients. The team then showed that clonally-expanded effector CD8+ T cells expressing CXCR6+ Granzyme B+ and interferon gamma+ are increased in individuals with thyroid adverse events. Furthermore, they found that IL-21 from CD4+ T helper cells drives the thyrotoxic function of these CD8+ T cells and that inhibition of IL-21 in a mouse model prevented checkpoint inhibitor-associated thyroid autoimmunity.
IMPACT
The findings highlight potential immune pathways that can be targeted to reduce immunotherapy toxicities in patients. Understanding how autoimmune toxicities develop in patients treated with cancer immunotherapy will help researchers develop strategies to reduce these side effects, making treatment safer.
In addition, mechanisms driving cancer immunotherapy-related autoimmunity may be shared with spontaneous autoimmune diseases, such as type 1 diabetes and Hashimoto's thyroiditis. Thus, findings from this study can also help researchers identify targets for the treatment of a broad number of autoimmune diseases.
JOURNAL
The online in the journal Science Translational Medicine.
AUTHORS
The study’s senior author is Dr. Maureen Su, professor of Microbiology/Immunology and Medical Genetics at UCLA. Both Dr. Su and Dr. Lechner are members of the UCLA Jonsson Comprehensive Cancer Center. Other UCLA authors include Zikang Zhou. Aline T. Hoang, Nicole Huang, Jessica Ortega, Lauren N. Scott, Ho-Chung Chen, Anushi Y. Patel, Rana Yakhshi-Tafti, Kristy Kim, Willy Hugo, Pouyan Famini, Alexandra Drakaki and Antoni Ribas.
JOURNAL
This work was supported in part by grants from the American Thyroid Association, the National Institutes of Health and the Aramont Charitable Foundation.