New Jersey resident Andre LaPierre, 67, thought he had put cancer behind him. In 2019, he was diagnosed with prostate cancer and had, what he thought, a successful surgery to remove his cancerous prostate.
But during a check-up in January of 2022, his doctor noticed that his PSA levels went up, even though they shouldn’t have. If PSA levels are elevated, it can indicate the presence of cancer.
He followed up by getting a prostate-specific membrane antigen (PSMA) PET scan, which showed a single small nodule — another potential sign of the cancer returning.
“My original surgeon said operating really wasn't the best way to go about treating this because the nodule was so small — only three millimeters — it would be like finding a needle in a haystack,” said LaPierre. “Instead, he suggested androgen deprivation therapy and radiation, which I wasn’t comfortable with. I just knew there had to be a better way.”
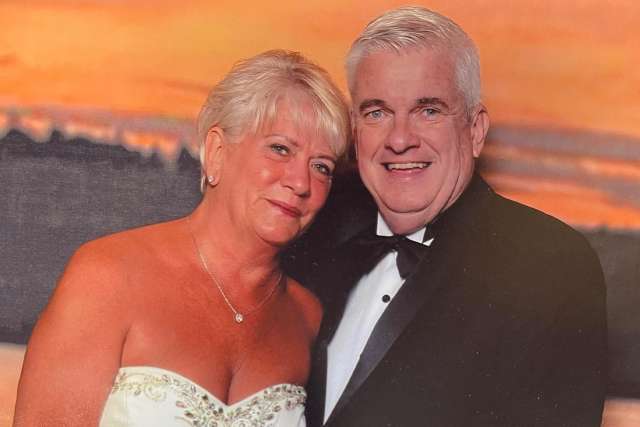
LaPierre, a successful real estate broker who has been married to his wife, Judy, for 43 years and is the father of three and grandfather to eight, decided to look for a second opinion and found himself going nearly 3,000 miles west to UCLA Health.

A novel approach found only at UCLA
After looking for potential clinical trials online, LaPierre saw a trial for a , which is being led by researchers Robert Reiter, MD, professor of urology and chief of , and Jeremie Calais, MD, associate professor and director of the Clinical Research Program of the .
“Historically, surgeons would look at the x-rays and then try to find the involved lymph node or lymph nodes by operating on the corresponding area,” said Dr. Reiter. “However, it turns out that 50% of the time they were not able to find and remove the involved lymph node. Thus, the need for surgical guidance intra-operatively.”
To help overcome the “needle in a haystack” issue, the UCLA team is now testing a novel approach using a PSMA tracer to help identify the involved lymph nodes and guide the surgery.
Patients in the trial are given a PSMA tracer, which is a small molecule tethered or conjugated to a radio isotope, which can be detected with a gamma probe to determine where the lymph node is located. So, if something lights up on the scan, the surgeons can find that in the operating room.
“So far, I'd say that we've identified the lymph node 95% of the time, and were able to successfully remove it,” Dr. Reiter said. “And the purpose of doing that, of course, is with the hope that maybe that’s all the disease that there is, and that it might be curative, or at a minimum, that it will delay the time until they need additional treatment.”
Choosing surgery
After talking to both Dr. Reiter and Dr. Calais, LaPierre knew this was the right treatment plan for him. He had his surgery set with Dr. Reiter for June 2022, just a few months after finding out about his small nodule.
The surgery went smoothly and LaPierre got the green light to go back on a plane to head home to New Jersey just two days later.
“When I came out of the surgery, my wife was in tears,” said LaPierre. “I thought for sure it was because something went wrong. But nope, it was because they were able to find the nodule and remove it.”
The lymph node ended up being located in an area where most urologists would not normally think to look for lymph nodes. It was a mesorectal lymph node, essentially a node in the fatty tissue around the rectum, which is an area that is not normally explored for prostate cancer.
“There's no way we ever would have found the lymph node without this technique,” said Dr. Reiter.
Moving forward
Now 17 months post-surgery, LaPierre’s latest PSA test came back less than 0.04, essentially undetectable.
“I can’t say enough about everyone at UCLA Health,” said LaPierre. “I had a million questions for Dr. Reiter and he took the time to answer every single one of them. I am so grateful to the entire UCLA medical community for the fantastic treatment and loving care I received.”
LaPierre said he is glad he took the time to find the right doctors and hospital that would listen to what he felt was important and find a treatment that was right for him.
“You have to do what’s right for you and be your own advocate,” said LaPierre. “If somebody's operating on you, and you're not sure what's going on and you're not confident, ask questions and bring people in with you to help. It’s your life, and you’ve got to do the research. I never would have found this study if I didn’t try to see what other options were available. This may not be the final answer in my journey, but it’s got me nearly two more years so far and hopefully more time.”
Take the Next Step
Learn more about at UCLA Health.