Fifteen years after being diagnosed with prostate cancer and having his prostate removed, John Babcock, now 68, watched with extreme concern as his prostate-specific antigen (PSA) test numbers continued to “climb and climb.”
Men generally have low levels of PSA protein in their blood stream, but if those numbers rise it could indicate an infection, inflammation, or cancer of the prostate.
In Babcock’s case, it seemed clear that his condition was getting worse, but the doctors in his HMO just shrugged, he said.
“Every time I would go in, they'd say, ‘Well, you know, it's going up, and if it doubles within a six‑month period, then we're going to have to do something,’” Babcock said.

He’d ask: “Why wait?”
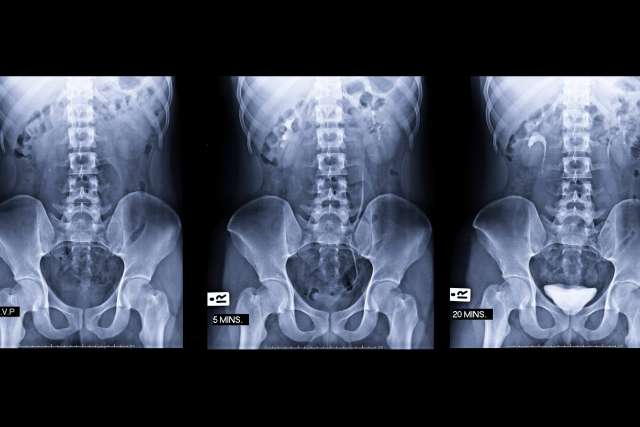
Finally, a change in insurance in 2018 allowed him to seek help at UCLA Health, where his primary care doctor suggested he sign up for the “SCIMITAR” study, which advances treatment options for prostate cancer with the use of short-course radiotherapy.
As part of the program, he received five high-dose radiation treatments over a two-week period, with each treatment taking less than an hour. His PSA level now? It’s nearly undetectable, Babcock said.
“I’m not saying I’m cured,” he said. “You have to wait five years before you’re officially cured. But it goes to show what smart doctors can do.”
Babcock said he learned about SCIMITAR from UCLA Health’s Sandy Ting Liu, MD, a board-certified physician in oncology.
"Dr. Liu said, 'I think I have something that will help you, but it's an experimental thing,'" Babcock said. "She asked if I would be willing to be a part of a new study. And, of course, I was like, 'You bet.'"
After months of hormone therapy to slow the progress of his disease, Babcock said he was "game for anything."
Liu said Babcock seemed to be the perfect candidate for UCLA’s cutting-edge radiation therapy.
“We have a robust prostate cancer program here at UCLA,” Liu said. “If a patient has high-risk disease we would intensify the therapy upfront. We believe the outcome is better.”
At Liu’s direction, Babcock set up an appointment with Amar U. Kishan, MD, chief of genitourinary oncology and vice chair of clinical and translational research in the Department of Radiation Oncology at the David Geffen School of Medicine at UCLA and the UCLA Jonsson Comprehensive Cancer Center.
"So I met with Dr. Kishan, and they did blood work and the usual stuff, and he says, 'OK. Well, let's do this thing,'" Babcock said.
Babcock said he had been told by doctors at another medical institution that his prostate cancer was incurable and he would need to be on hormone therapy the rest of his life. Dr. Kishan disagreed.
"We determined that he very likely has a curable form of prostate cancer, where we can get him off the hormone therapy and treat with radiation," Dr. Kishan said.
Babcock went in for five radiation treatments over a two‑week period. "Each treatment took maybe at most an hour," he said.

He also was able to give up hormone therapy – which had substantially affected the quality of his life.
"You know, there are side effects to these hormone shots that are rather unpleasant," Babcock said. "You get hot flashes. You get moody. They call it 'manopause.'"
A little over a year has passed since Babcock's last treatment, and so far there is no sign that the cancer has returned.
"Talking to Dr. Kishan, he says he’d be very surprised if it came back but we’re going to monitor it for the next five years,” said Babcock, adding that he visits UCLA Health for check-ups every six months.
He wants other men to know that there are new treatment options for a cancer that claims nearly 35,000 lives each year in the United States.
“Here I am, a little over a year later, and the cancer’s not there,” Babcock said. “I don't want to get, you know … no false promises here. But I'm fine.”
Learn more about Radiation Oncology services at UCLA Health.
Tina Daunt is the author of this article.
Related articles
Genetics, technology are improving radiation treatment for prostate cancer
Advances in radiation technology help physicians deliver more precise and effective cancer treatment
'No early warning signs': It's important to keep up with prostate cancer screenings