ADC Stories
Personal Stories from the ADC Program: Meet Our Patients, Caregivers, and Staff
UCLA's award-winning Alzheimer's and Dementia Care (ADC) Program helps patients living with dementia and their caregivers meet the complex medical, behavioral, and social needs.
This program is a lifeline, providing emotional, educational, and medical support for patients living with this progressive disease and caregivers navigating the journey.
The ADC Program team tailors care for the patients, caregivers, and their families while learning about their life stories, joys, and hopes.
Meet some of the ADC Program's wonderful patients, families, and staff.
Patient Profiles
Meet Mary, a dynamic woman who wanted us to know that as a patient with memory loss, her sound advice is to always stay connected with your family. Mary emphasized enjoying and relishing with her family because, as she adds, "you never know how much time you have left together." We learned from Mary and her family that they are in contact often and remain a constant in her life. Dementia is a disease that can take away from patients and families, but after listening to Mary, it's evident that dementia can also bring patients and families closer together.

Hello, my name is Mary. My daughter Brigitte and I have been a part of the ADC program for almost 3 years.
What do you remember most about your childhood?
I was born in North Wales, England in 1934. Growing up, I remember my experiences during World War II, where people were given food rations and each family was given food coupons every week. We lived in the country and around farms, so we were lucky because there was always food and we were never hungry. I remember people being kind and looking out for one another.
How did you meet your spouse? What did you like about him?
I remember the day I met my husband, Peter. We met at a dance in Chelsea, London, after both of our friends stood us up. From the beginning I liked him right away, even though he had a terrible car. There was just something about him. Looking back, meeting my husband was the happiest moment of my life.
What were your happiest moments as an adult?
After we were married, we rented an oceanside apartment in Malibu for $125 a month. My most precious memories of that time are about raising our wonderful kids: Brigitte, David, and Lynda. It was a lovely time in our lives. I’m incredibly proud of my 3 children, who have turned out beautifully and are loving people.
What is one piece of advice you would give to the younger generation?
Stay connected with your family. Keep them together. Enjoy and love being with them, because you never know how much time you have left.
What advice would you give to other caregivers taking care of persons living with dementia?
Brigitte: Be patient. We all get caught up in our lives. Take the time and be patient. Ask the questions. Appreciate the time you have. We appreciate the time we have for each other. Time is limited so take advantage of that time.
Caregiver Profiles
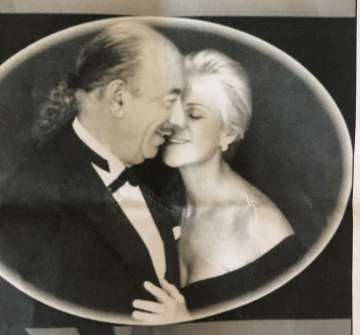
Sam and Paula were the epitome of a couple who lived their life to the fullest. From traveling the world, raising their blended families, maintaining close friendships, and playing competitive backgammon, these two never seemed to stay still. Throughout the ups and downs of the disease, they hardly left each others' side.
Tell us about Sam and what he meant to you.
Sam is my late husband and he meant everything to me. We were passionately married for over 40 years, and he filled my life with such joy and pleasure. It was a second marriage for both of us and he was a sweet and adoring father to my children. As a wife, I always felt that his main goal was to make me happy. I always felt cherished and loved.
If there is anything the world should know about Sam, what would it be?
Sam was glamorous, worldly, handsome, and well-dressed. That was evident to anyone who knew him. But I want people to know that he was kind and generous, had a very giving heart and a good soul. He was kind to everyone.
Tell us about your journey as a caregiver. How did you deal with the challenges you faced as a caregiver?
It was very hard seeing the person I loved becoming frail. The caregiving role came in baby steps and stages, happened over a few years. The main challenge for me was sadness. I had to overcome my sadness seeing the person I loved changing in front of me.
My family played a big role in helping me cope because they were around all the time. They were here almost every day and their presence helped a lot. As a caregiver, you must find ways to reach out to someone, whether it’s a support group, your family, and friends. You might be embarrassed to reach out, but you need to learn how to say “I need help. Can you come over for a few hours?”
As a caregiver, you must make sure your mental health is strong so you can take care of your loved one. As much as I loved him, it became difficult at times. I had to learn how to go to a place of love and show him more love than ever.
What advice would you give other caregivers taking care of persons living with dementia?
Sometimes we don’t have a choice on whether we want to take on this caregiving role. I would advise you to develop a sense of patience. Looking back, there were times when I could have been more patient because I was looking for the old Sam. Try your best to look for the person you know and remember the person you love. That person is still in there. Slow down and take it easy. Live in the moment. Get help and support. Reach out.
What silver lining have you found in this experience?
It made me feel happy to set an example for our children and grandchildren. The silver lining, I am passing on to them is how to have compassion. During our journey, our children and grandchildren became very compassionate people. Sam and I are passing that down as part of our heritage.
Eileen and Kevin have participated in the ADC program for over a decade. Through all the ups and downs of his mother's disease, Kevin has learned tremendous coping skills as he became the primary caregiver for his mother Eileen.
Tell us about your journey as a caregiver.
It started 7 years ago when our family noticed some minor symptoms of dementia. She started seeing a neurologist and was initially diagnosed with Mild Cognitive Impairment; however, the diagnosis later became Alzheimer’s dementia. During this time, I became proactive with educating myself and connecting with geriatric specialists.
What are some things you wish you would’ve have known in your journey as a caregiver?
There isn’t an “easy” way to get through this. I sought out whatever resources I could find, attended all the educational presentations and caregiver support groups. Having that information and that knowledge empowered me to make better decisions for myself and my Mom.
What are the most valuable lessons you learned as a caregiver?I have come a long way in my journey as a caregiver. First, I learned that I had to be the point person for my Mom’s care. Second, you need a specialty team to take care of the patients with dementia and their families. Third, if you are the child of the patient, the “role reversal” will be an ongoing process. Your lifelong relationship with your parent needs to switch, because you now need to look after them. The dynamic has to change because dementia is an irrational disease.
What advice would you give other caregivers taking care of persons living with dementia?
Seek out all the resources because many of them are free. Take care of yourself. It’s easy to put our own needs aside when we are busy taking care of our loved one, but you need to take care of yourself to take care of the person with dementia. Attend support groups so you can learn how to become a caregiver for the long term. These resources taught me that I am not alone in this journey and others have gone through it successfully.
Who is dad and what does he mean to you?
My dad means a lot to me. He was a significant mediator and harmonizing force within our family, bringing peace and tying our family together. As a father, he is noble, generous, and kind. My father is an excellent benchmark of expectations I have for other people.
Professionally, my father was an aerospace engineer, always having pens in his shirt pocket. Dad had an extensive career, working in Italy and contributing to Italian aerospace technology. Beyond his Science, Technology, Engineering, and Mathematics (STEM) expertise, he also loved the arts. He was immersed in the arts, having done folkorico dancing and speaking seven languages. He had a lot of dimensions to him, and he still does.
How did you deal with the challenges you face as a caregiver?

As a teenager, I began to see changes in my father, and he was diagnosed when I was in college. Since I was not with him daily, some of the changes were more noticeable. I am still learning how to be a caregiver. With the challenges that come, it is vital to adapt and be flexible in confronting the changing needs as things progress.
What are the most valuable lessons you learned as a caregiver?
Patience is a big one. You have to accept that some days are good and some are bad, nonetheless you are better at adapting to certain challenging situations. As a caregiver, you have to be emotionally flexible, restraining yourself and your emotions. In some cases, you may have to remove yourself from a situation and take time to step away even for a few minutes.
What advice would you give other caregivers taking care of persons living with dementia?
Dementia is a pervasive disease. It is helpful to know what the disease is about and how it affects people and their loved ones. Being a caregiver for someone with dementia can be an isolating experience; however, it is important to have avenues of support such as support groups, caregiver boot camps, counseling, and consulting with dementia specialists. I also found it helpful to learn how to educate others about what is happening. If someone is willing to learn more, lean into it and take those moments as you go.
Staff Profiles
Dr. David Reuben is the Director of the Multicampus Program in Geriatrics and Medicine and Gerontology, Division Chief of Geriatrics at UCLA, Archstone Foundation Chair, Professor at the David Geffen School of Medicine at UCLA, and the Director of the UCLA Alzheimer's and Dementia Care Program. Dr. Reuben started the ADC Program at UCLA and has pioneered nationwide dissemination.
Tell us about your journey to get to the ADC program.
My journey for ADC began about 25-30 years ago, when I started to research how to improve the care for older people in healthcare systems through quality improvement, physician education, and practice redesign. Over time, I learned that if taking care of patients with dementia was a health care professional’s (dedicated) job, perhaps it might get done properly. I spent time with other program developers and became convinced that the most appropriate person for the Dementia Care Specialist role would be an Advanced Practice Provider such as a nurse practitioner.
What made you decide to want to work with older adults?
This decision goes back to when I was a young faculty member at Brown University. I was teaching general internal medicine at the time. My fiancée was doing additional training and coming back at the end of every day feeling happy about what she was learning. I decided to get further specialty training. My department chair recommended that I consider geriatrics. I spoke to as many geriatricians as possible and they all told me they never regretted going into geriatrics. In 1987, I took a sabbatical at UCLA and fell in love with geriatrics and Los Angeles. I’ve never looked back.

What do you find most rewarding about the ADC program (patients, caregivers, ADC accomplishments, co-workers)?
The ADC team. It is an entity that makes decisions and moves forward, sees needs and comes up with solutions. It has become a true program, a cohesive group of individuals who have eyes on the same prize and work together to get things done.
What hobbies/interests do you have outside of work?
I take care of myself with exercise such as yoga, swimming, and running. I also like to write plays and lyrics to songs. Plus there’s always baseball.
What gives you satisfaction in your work?
It makes me happiest to see the ADC team and other faculty members helping people by providing the right care.
How has your passion for patient care evolved? What is your favorite thing that you take home?
It has deepened from my younger days. I learned that the relationship between the patient, clinician, and family has to be individualized. Even in dealing with the same diseases, it’s about respecting the patient and their choices, helping them achieve what they want. For some patients, they want to get walking again. For others, they are ready for the last chapter of their lives.
What is your biggest hope for patients and families living with dementia?
My greatest hope is that anyone living with dementia is able to get comprehensive care, and that access isn’t constrained because there of their inability to pay for it.
What advice would you give for medical providers who are interested in pursuing this field?
It takes a team. You can’t take ownership of everything for 2 reasons: there isn’t enough time and there are other people that are experts. In my practice of medicine and in about anything I do, it is very much a team approach and we work together to achieve common goals. Also, use your voice to bring up problems that need to be solved.
Dr. Michelle Panlilio has been a part of the UCLA ADC program for over a decade, working with countless patients and caregivers living with dementia. She serves as the National Lead Dementia Care Specialist, disseminating the ADC program into healthcare systems nationwide. Michelle is passionate about working in dementia care, with interest stemming from a young age caregiving for her grandmother. Dr. Panlilio started the ADC Profiles project to showcase who our patients, caregivers, and staff are beyond the disease.
Tell us about your journey to get to the ADC program.
I started wanting to learn more about dementia when I was 13. That's when I became the primary caregiver for my grandmother. Growing up, I knew I wanted to do something for patients with dementia, but I did not know what. As far as my journey to the ADC, it was not always clear cut since my background clinically was with internal medicine and research/clinical trials. After being offered positions in oncology and the ADC program, I ultimately decided to pursue a career in dementia.
How has that passion evolved? What is your favorite thing that you take home?
My passion for our patients has strengthened and diversified over time, as I learned more about the challenges they face with their caregivers. We have the best patients and caregivers on the planet. No matter how advanced the disease is, I still learn something new every day from our patients and caregivers. The more that I work with them, the more I learn—whether it is to be a more compassionate clinician or a better human being.

What do you like best about the ADC?
Aside from our patients, it’s our team. I have never met more motivated, compassionate people who want to provide our patients and families with the best care. There is nothing glamorous about what we do and we are dealing with a progressive disease, yet everyone on this team is determined to put their best effort to do the right thing for our patients and caregivers.
What is your biggest hope for the ADC program?
I have 2. My biggest hope for the ADC program is to continue to grow the program nationwide and provide more care for patients and families living with dementia. Another hope is for patients and families to access services and resources at no additional cost. Our patients are our nation's elderly - they have taken care of us and we need to take better care of them.
How do you keep going when things get tough?
What keeps me going is focusing on the goal, which for me has always been to provide the best care for patients and their families. I rely heavily on our team for support. When I have no energy left, there is always someone on my team willing to lend a hand.
What hobbies/interests do you have outside of work?
My family keeps me in check and sane. They are wonderful reminders of what truly matters most. At the end of the day, they are my heroes. Aside from my family, I do something good for myself daily- which usually involves exercise like power yoga, running, Peloton, and lifting weights. I do that to take care of myself, because it forces me to be more mindful of the people and events around me.
What’s a fun fact about you/what is something on your bucket list?
A fun fact about me is that I married my high school sweetheart. Our first unofficial date was at In-N-Out Burgers!