Clinically Non-Functioning Pituitary Adenomas
Find your care
We treat pituitary tumors using the latest innovations in minimally invasive procedures. To connect with an expert in the pituitary tumor program, call .
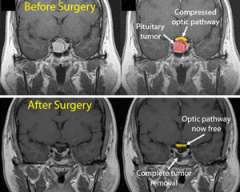
Pituitary tumors (adenomas) that do not secrete active hormones are called clinically nonfunctioning pituitary adenomas. Most are large (macroadenomas), measuring more than one centimeter in size at the time of diagnosis. Patients start experiencing symptoms when the large tumor compresses the optic nerves, leading to vision loss, or the loss of normal pituitary function.
Clinically Nonfunctioning Pituitary Adenomas: Expert Care in Southern California

The UCLA Pituitary Tumor Program offers comprehensive management of clinically nonfunctioning pituitary adenomas. Our physicians have years of experience in diagnosing, treating and managing pituitary conditions.
Use these links to explore more about clinically nonfunctioning pituitary adenomas:
Clinically Nonfunctioning Pituitary Adenomas: Causes
Clinically nonfunctioning pituitary adenomas make up about half of pituitary adenomas. The vast majority of them are benign.
There are several possible reasons why nonfunctioning pituitary adenomas could occur:
- Typically, the body produces hormones by taking a larger molecule and cutting it at the right places to create a functioning hormone. In some cases, something is wrong with this cutting process and a "functional" hormone is not made. The hormone might still travel into the bloodstream, but it is inactive and usually cannot be detected using standard blood tests.
- In some cases, the hormone might be formed inside the cell, but there is something wrong with the transport process that is required to release it into the blood stream.
- In other cases, the tumor cells simply do not produce a hormone
Clinically Nonfunctioning Pituitary Adenomas: Symptoms
The most common symptoms are due to the large tumor compressing nearby structures, leading to:
-

Vision loss
- When large pituitary adenomas (macroadenomas) grow upward into the brain cavity, the tumor can elevate and compress the optic chiasm.
- A loss of the outer peripheral vision, called a bitemporal hemianopsia
When severe, a patient can only see what is directly in front of them; many patients do not become aware of their visual loss until it is quite severe.
- Other visual problems include:
- Loss of visual acuity (blurry vision), especially if the macroadenoma grows forward and compresses an optic nerve
- Inability to perceive colors as brightly as usual
Pituitary Failure or Hypopituitarism
Increased compression of the normal gland can cause hormone insufficiency, called hypopituitarism. The symptoms depend upon which hormone is involved.
- Reduction of sex hormones, luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
- In men, this can lead to a low testosterone level, causing decreased sexual drive and impotence.
- In some cases, there can be loss of body and facial hair.
- In women, this can lead to infertility.
- Large pituitary tumors can slightly elevate blood prolactin levels. Doctors think this occurs because of compression of the pituitary stalk, the connection between the brain and the pituitary gland. It is called the "stalk effect."
- In premenopausal women, this can lead to reduction or loss of menstrual periods and/or breast milk production (galactorrhea).
- Prolactin levels are only slightly elevated, as opposed to prolactinomas in which the prolactin level is usually very high.
More severe hypopituitarism can lead to hypothyroidism or abnormally low cortisol levels, which may be life threatening. Symptoms of severe hypopituitarism include:
- Loss of appetite
- Weight loss or weight gain
- Fatigue
- Decreased energy
- Decreased mental function
- Dizziness
Changes in hormonal function can cause electrolyte imbalance in the blood, typically low sodium levels (hyponatremia). Symptoms could include:
- Fatigue
- Seizures
Clinically Nonfunctioning Pituitary Adenomas: Diagnosis
Imaging scans are one method doctors use to diagnose clinically nonfunctioning pituitary adenomas. We will also order hormone tests to evaluate the levels of pituitary hormone, confirming that there is no evidence of hormone production by the tumor.
Your doctor will conduct a thorough physical examination and ask you about your symptoms and medical history. He or she will then order tests as necessary, including:
- Magnetic resonance imaging (MRI) scan
- Hormone test
- Vision test
MRI Imaging
MRI imaging allows us to detect whether there are tumors present. Your doctor will use a special MRI pituitary protocol to best visualize the tumor.
There are other tumors that produce symptoms similar to that of a pituitary adenoma. Your doctor will want to rule out these other tumors before confirming a diagnosis. Tumors that mimic the symptoms of a pituitary adenoma include:
- Craniopharyngioma
- Rathke's cleft cyst
- Meningioma
- Arachnoid cyst
- Granulomatous diseases
- Glioma of the suprasellar region
- Metastatic tumor
- Chordoma

Hormone Testing
If your symptoms suggest pituitary failure (hypopituitarism), your doctor may order a complete evaluation of the endocrine system. Based on results of these blood tests, you may undergo additional hormonal studies.
Learn more about hormone testing at the UCLA Pituitary Tumor Program.
Visual Testing
If you are experiencing vision problems, your doctor will recommend that an experienced ophthalmologist evaluate you. The evaluation should include:
- Acuity testing of each eye
- Formal visual field testing
This will determine if you have a loss of peripheral vision.
Clinically Nonfunctioning Pituitary Adenomas: Treatment Options

The UCLA Pituitary Tumor Program offers comprehensive management of all types of pituitary tumors. Treatment options for pituitary adenomas include:
- Surgery
- Medication
- Radiation Therapy
Surgery for Clinically Nonfunctioning Pituitary Adenomas
For most patients with nonfunctional adenomas, surgically removing the adenoma is the most effective treatment.
Whether this will lead to a long-term cure depends on the extent of surgical removal, which is related to:
-
Tumor size
- If the tumor invaded the cavernous sinus (the compartments on either side of the pituitary sella)
- If the tumor expanded into the brain cavity
- The experience and expertise of the operating surgeon
If the surgeon was able to remove the entire tumor, the cure rate is 70 percent to 80 percent. Overall, surgery improves:
- Vision in 75 to 90 percent of patients
- Headache in 80 to 90 percent of patients
- Suppressed pituitary function in 10 to 30 percent of patients
If the pituitary adenomas require surgery, typically the best procedure is through a nasal approach. Our neurosurgeons who specialize in pituitary tumor surgery are experts in the minimally invasive endoscopic endonasal technique. This procedure removes the tumor while minimizing complications, hospital time and discomfort. This advanced technique requires specialized training and equipment.
Very large tumors that extend into the brain cavity may require opening the skull (craniotomy) to access the tumor. Our surgeons are also experts in the minimally invasive "key-hole" craniotomy, utilizing a small incision hidden in the eyebrow.
If, after your surgery, some tumor cells remained or regrew, you may be a candidate for radiation therapy or a repeat surgery.
Medication for Clinically Nonfunctioning Pituitary Adenomas
Hormone replacement may be necessary if you have pituitary insufficiency.
Radiation Therapy
Doctors may recommend radiation therapy as a second-line therapy for endocrine-inactive tumors. Focused-beam radiation, named stereotactic radiosurgery, can be effective in controlling tumor growth. In some cases, radiation therapy may cause a loss of pituitary function.
Contact Us
To schedule an appointment with one of our physicians at the Pituitary Tumor Program, please call .
You can also email us at