Phrenic Nerve Repair
Find your care
Our team is made up of experts and leaders in the art and science of plastic surgery. To learn more about our services, call .
The Phrenic Nerve Program is a collaboration between at the UCLA Division of Plastic & Reconstructive Surgery and at the . For more information or to schedule a consultation, please call (855) 233-3681.
The phrenic nerve controls function of the diaphragm muscle - the primary muscle involved in breathing. It tells the diaphragm when to contract, allowing the chest cavity to expand and triggering the inhalation of air into the lungs.

Injury to the phrenic nerve can impair the ability of the nervous system to regulate breathing. It is known risk associated with chest and neck procedures such as coronary bypass surgery (CABG), neck dissection for head and neck cancer, surgery of the lungs, heart valve surgery, surgery of the aorta, thymus gland surgery, carotid-subclavian bypass surgery, and surgery for thoracic outlet syndrome. The phrenic nerve can also be injured by epidural injections, interscalene nerve blocks, and even chiropractic manipulation of the neck.
In the past, treatment options for phrenic nerve injury were limited to either nonsurgical therapy or diaphragm plication, neither of which attempts to restore normal function to the paralyzed diaphragm. Patients endured chronic shortness of breath, sleep disturbances, and lower energy levels. They were often told by their physicians that they would simply have to live with it.
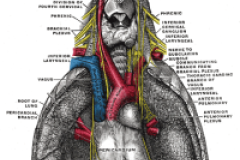
Advances in nerve decompression and transplant allow reconstructive plastic surgeons to reverse diaphragm paralysis. The techniques used are derived from the procedures commonly used to treat arm or leg paralysis, which have allowed surgeons to restore function to previously paralyzed muscle groups.
The rarity of the condition often makes it difficult for patients with a phrenic nerve injury to find treatment. The condition is often mis-diagnosed or viewed as insufficiently severe enough to require corrective surgery.
Patients who have undergone phrenic nerve surgery report improvements in their physical and respiratory function, and a reversal of the sleeping difficulties related to diaphragm paralysis.
If you have been diagnosed with a paralyzed diaphragm, you may be a candidate for phrenic nerve repair. In order to expedite your inquiry, please have the following information ready:
- When were you diagnosed with a paralyzed diaphragm (month/year)?
- What side(s) of your diaphragm is paralyzed?
- Did you have surgery or trauma that caused damage to your phrenic nerve?
- Do you experience numbness and/or tingling in your upper extremities?
- When was your most recent SNIFF (Chest Fluoroscopy) test completed?
- When was your most recent Pulmonary Function Test completed?
- Have you had an EMG nerve study completed of your phrenic nerve and diaphragm?
Related Articles:
Kaufman, MR et al. Chest 2011;140;191-197
Kaufman, MR et al. Clin Neurol Neurosurg (2012), doi:10.1016/j.clineuro.2012.01.048
About the Doctors:

Reza Jarrahy, MD
Reza Jarrahy, MD earned his bachelor's degree from Stanford University and his medical degree from the State University of New York's Stony Brook School of the Medicine. He completed his general surgery training at New York University and University of California, San Diego, and completed his plastic surgery residency at the David Geffen School of Medicine at UCLA. He elected to complete an additional year of sub-specialty fellowship training in craniofacial surgery at David Geffen School of Medicine at UCLA before joining the UCLA Division of Plastic & Reconstructive Surgery as an assistant professor in 2007. Dr. Jarrahy specializes in the care of pediatric patients with rare and complicated craniofacial disorders. He travels abroad on an annual basis to assist in the care of craniofacial patients in Brazil and Guatemala.
Dr. Matthew Kaufman is an award-winning cosmetic and reconstructive plastic surgeon, board certified in both Plastic Surgery and Otolaryngology-Head and Neck Surgery, and he is a Fellow of the American College of Surgeons (FACS). Dr. Kaufman embarked on his surgical training at one of the nation's top training programs for Otolaryngology - Head and Neck Surgery at The Mount Sinai Hospital in Manhattan. He continued his training in Plastic and Reconstructive Surgery at the prestigious UCLA Medical Center in Los Angeles. Among his nerve surgery expertise which he performs together with his partners at the Institute for Advanced Reconstruction in Shrewsbury, NJ, Dr. Kaufman is the only known surgeon to perform specialized phrenic nerve surgery. He has patients worldwide, including from Australia, Canada, Israel and one scheduled from Ireland; 11 is the youngest he has operated on for phrenic nerve problems, and early 70s the oldest.