Racial disparities in infant health have persisted for decades, with people of color at increased risk for poor health outcomes, including preterm birth (born before 37 weeks) and low birth weight (less than 5.5 pounds). Both have long-term effects on neurodevelopment, and preterm birth is a leading cause of infant mortality.
In 2019, nearly 450,000 babies were born in California. Some of these new lives were already touched by inequity: preterm birth rates were 67% higher for Black parents than white parents. Latinx and Asian rates were 36% and 11% higher, respectively. Increased rates were also present for term-birth low birth weight: 150% higher for Black; 38% for Latinx and 81% for Asian.
In a new study, researchers examined how neighborhood environments accounted for disparities in infant health outcomes in California’s 2019 birth records data. They measured the impacts of air pollution, drinking water contamination, green space (tree canopy coverage), heat vulnerability and noise. They also looked at the “area deprivation” factor – an aggregate measure of neighborhood income, education, employment and housing quality.
Highlights of their findings included:
- Black/Latinx vs. white disparities were due to area deprivation.
- Air pollution was a significant factor in the Latinx vs. white disparity in term-birth low birth weight.
- Lack of greenspace was a factor in Black, Latinx and Asian disparities.
The study noted that Black and Latinx birth parents generally lived in the most disadvantaged neighborhoods compared to white and Asian counterparts.
“I'm always interested in the mechanisms of racism,” said Shiwen “Sherlock” Li, PhD, first author of the study, “and how different racial groups get differential treatment because of the distribution of green space, industrial power plants or road construction. There is ritualized policy that's behind all these mechanisms, creating these health disparities down the road.”
“This study supports the call for further improvements in cleaning our air and drinking water and increasing access to green space in urban environments, especially in neighborhoods where Black and Latinx communities reside,” said Beate Ritz, MD, PhD, the study’s senior author and a professor in the department of epidemiology at the UCLA Fielding School of Public Health, and in the department of neurology at the David Geffen School of Medicine at UCLA.
Mediation analysis
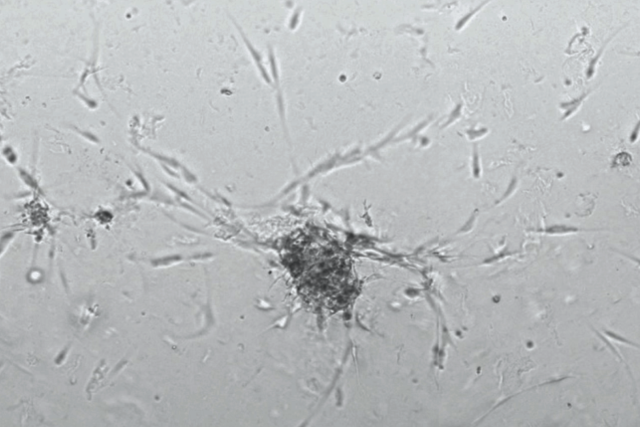
Dr. Li and his colleagues employed mediation analysis, a widely used tool in epidemiology. It allows them to examine how one variable (membership in racial categories) influences another variable (birth outcomes) through mediators (environmental factors) that underlie that pathway.
The birth parents’ residential addresses allowed the researchers to map neighborhoods at the census tract level and their corresponding environmental data, such as annual average particulate matter (PM2.5), drinking water quality and tree canopy coverage.
But infant health outcomes result from a wide range of elements – so the researchers’ analysis had to parse out non-environmental risks. These were socioeconomic and behavioral characteristics found at the individual level in the birth records data. They included, for example, adequacy of prenatal care; public or no health insurance; smoking during pregnancy; chronic or gestational diabetes; and hypertension.
Dr. Li worked with Roch A. Nianogo, MD, PhD, MPH, an assistant professor of epidemiology at the school of public health, to devise complex computational models that controlled for all the individual risks and focused just on the pathway of race to neighborhood environment to birth outcome.
Environmental justice
Dr Li’s passions for environmental sustainability and understanding racial disparities began as an undergraduate at the University of California San Diego. He observed disparities in users of the Triton Food Pantry, where he volunteered for two years as a manager helping provide emergency food relief for students.
He was in the midst of his graduate work in Parkinson’s disease at the school of public health when the department of epidemiology awarded him a scholarship in 2020. “HEALRISE” (Health, Racism, Inequities and Social Epidemiology) provided funds for the birth outcomes study.
“I wanted to look at taking some of the blame and responsibilities off the individual level and more on improving environments,” said Dr. Li, now a postdoctoral scholar at the University of Southern California. “In my opinion, it's more approachable to address health disparities through policy changes.”
Dr. Li noted that raising neighborhood-level incomes or education is difficult. But he believed that air pollution, drinking water quality and green space were all more easily tackled, especially the last one.
“I went to a couple of community meetings and people always wanted more green space,” he said. “This study adds to the proof that we need more equitable distribution of green space.”
Dr. Li hoped further studies would provide more understanding of the environmental factors that impact health disparities. For example, better measures and data for noise levels and vulnerability to extreme heat would help researchers and policymakers understand their impacts.
“Also, any of the variables – green space, heat, air pollution -- all interact with each other,” he said. “We need more complicated methods to model the interactions among the different environmental factors.”