Scientists at the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA have received more than $17.4 million in grants from the California Institute for Regenerative Medicine, the state’s stem cell agency, to advance new stem cell-based treatments for heart disease, ovarian cancer and a creatine deficiency disorder.
Targeted drug therapy for heart disease
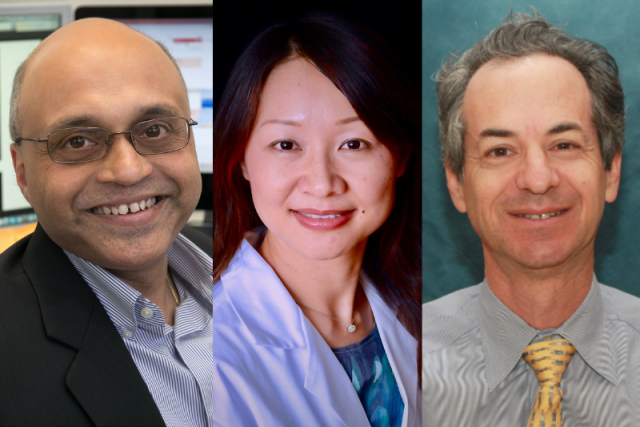
Dr. Arjun Deb, professor of medicine and molecular, cell and developmental biology
Deb’s $6 million clinical-stage research award will advance a new treatment for heart attack and heart failure. Cardiovascular disease is the leading cause of death globally, accounting for approximately one-third of all deaths worldwide. After a heart attack, the heart muscle dies. There are currently no therapies that improve the heart’s repair process after a heart attack, which is the leading cause of heart failure.
To halt this predictable but vicious progression, Deb and his team have engineered a therapeutic monoclonal antibody, a type of targeted drug therapy, that enables the heart to repair better and prevents the development of heart failure after heart attacks. The antibody targets a specific ectonucleotidase and a single dose has been shown in preclinical studies to prevent scar tissue formation and enhance cardiac function after a heart attack. Now, this new grant will help Deb’s laboratory scale up manufacturing of the drug product and continue research on the therapy’s safety and efficacy in larger animal models. The team will complete all preclinical testing required to submit an Investigational New Drug application to move the project to a phase 1 clinical trial in one to two years.
Off-the-shelf immune cell therapy for ovarian cancer
Dr. Lili Yang, professor of microbiology, immunology and molecular genetics
Yang’s $6.3 million translational research award will fund the development of a new off-the-shelf immune cell therapy to treat ovarian cancer by engineering blood stem cells to produce potent chimeric antigen receptor-armed invariant natural killer T cells, or CAR-NKT cells. While conventional CAR-T cell therapies have revolutionized the treatment of specific blood cancers, efforts to apply therapies of this kind to treat solid tumors have had limited success. This is due in part to solid tumors’ ability to evade CAR-T cell attack and to create tumor environments that suppress CAR-T cell activity.
To overcome this limitation, Yang’s laboratory has created . NKT cells are the special forces of the immune system that can attack a solid tumor using multiple weapons to prevent its immune evasion. These special immune cells can also selectively and effectively deplete the most immunosuppressive cells in its surroundings. As a result, this platform has the potential to target solid tumors like ovarian, brain and liver cancer. Collaborating with gynecologic oncologist Dr. Sanaz Memarzadeh, bioinformatician Dr. Matteo Pellegrini and biostatistician Dr. Jin Zhou, all of the UCLA Health Jonsson Comprehensive Cancer Center, Yang and her team will use the new funding to complete the research necessary to initiate IND-enabling preclinical studies, bringing the off-the-shelf CAR-NKT cell therapy a step closer to a clinical trial for the treatment of ovarian cancer, the deadliest cancer of the female reproductive system.
Gene therapy for creatine deficiency disorder guanidinoacetate methyltransferase deficiency
Dr. Gerald Lipshutz, professor of surgery and molecular and medical pharmacology
Lipshutz’s translational research award of $5.1 million will support his development of a gene therapy for guanidinoacetate methyltransferase deficiency, or GAMT, a rare creatine deficiency disorder that commonly results in intellectual disabilities, issues with speech, involuntary movements and recurrent seizures. Creatine is a substance that helps the brain and muscles store and produce energy. The only currently available treatment for this inherited disorder focuses on a strict diet of high-dose creatine, which is minimally effective and leaves some patients at risk of recurrent seizures and other symptoms.
In extensive preclinical studies in mice, Lipshutz and his team have shown that a viral vector-based gene therapy they developed , which accumulates with this disease. The team will be using the new CIRM grant to prepare a pre-IND package submission to the U.S. Food and Drug Administration, setting up this gene therapy to be evaluated in humans in a phase 1 clinical trial.