Prostate Cancer – Brachytherapy
Find your care
Radiation oncologists use a patient-centered approach and individualized treatment plans. To learn more and make an appointment with a UCLA radiation oncologist, contact us at:
Westwood -
Santa Clarita -
Santa Monica -
Here, at the UCLA Radiation Oncology Division of Brachytherapy, we are committed to making your cancer treatment a comfortable and successful experience. With over 30 years of experience (over 4,000 prostate implants), we have some of the most expertise and best published results on the use of HDR Brachytherapy for prostate cancer in the nation.
What is HDR Monotherapy and Combination therapy?
There are two forms of brachytherapy performed for the treatment of prostate cancer:
- Low dose rate (LDR) in the form of permanent seeds
- High dose rate (HDR) temporary implants
HDR temporary implants are performed both as a stand-alone treatment known as "HDR monotherapy" or used in combination with external beam radiation therapy (EBRT) as part of “Combination” therapy.
HDR is performed using a single tiny (1mm x 3 mm) highly radioactive source of Iridium-192 that is laser welded to the end of a thin, flexible stainless steel cable. The source is housed in a device called an afterloader. The computer-guided afterloader directs the source into the treatment catheters placed in and around the prostate by the brachytherapy physician. The source travels through each catheter in 5 mm steps, called “dwell” positions. The distribution of radiation and dose is determined by the dwell positions the source stops at and the length of time it dwells there. This ability to vary the dwell times is like having an unlimited choice of source strengths. This level of dose control is possible only with HDR.

Choosing HDR brachytherapy as a treatment
There are many advantages to HDR brachytherapy for treating prostate cancer which include:
- Safely escalating the dose to the tumor while minimizing the dose to the surrounding normal organs (ie rectum, bladder, and urethra)
- Ability to shape the radiation dose to fit the tumor and avoid normal tissues
- Minimize areas of radiation overdose (hot spots) or underside (cold spots) within the prostate
- Ability to adequately cover tissue immediately beyond the prostate (ie extracapsular extension)
- Free-hand technique allows a larger number of patients to be candidates for HDR as pubic arch interference and/or extracapsular/seminal vesicle involvement can be easily managed
- The high dose per treatment takes advantage of the unique biology of prostate cancer
- Accurate and precise delivery of the radiation dose before radiation treatment is given
- Organ motion (target movement) is not an issue as the target moves with the implant
- No radiation source (seed) migration to other organs
- No radiation exposure to other people
- Short course of treatment measured in days to weeks rather than months (as with permanent seeds or external beam radiation therapy)
- Fewer urinary effects compared with low dose rate seeds
- Shorter duration of androgen deprivation therapy (ADT) when ADT is used
- Effective treatment for patients with prostate cancer recurrence (“salvage” therapy)
Choosing UCLA for HDR brachytherapy
Our group performed hundreds of LDR implants before switching to HDR in 1991. We were one of the first centers in the USA to use high dose rate (HDR) brachytherapy to eradicate tumors. We feel that HDR temporary implants are superior to permanent seeds implants in most circumstances. To date, our center has done over 4,000 HDR brachytherapy implants for prostate cancer and is one of the most experienced centers in the nation.
We first started our HDR prostate program using HDR as a boost in combination with external beam radiation therapy. Our published results on patients followed for 10 years are among the best reported in the literature (1).
Our HDR monotherapy prostate protocol was developed in 1996 for patients who were not candidates for combined HDR and external beam radiation therapy. We observed that HDR Monotherapy for prostate cancer was a safe and effective treatment and thus began our HDR Monotherapy program. We have treated over 500 patients with HDR Monotherapy and it is now a routinely recommended treatment option at UCLA and worldwide. Our 10 year results have shown excellent clinical control of disease and few side effects (2).
Today, UCLA Division of Brachytherapy continues to be leaders in HDR techniques for the treatment of prostate cancer. Members of the Division serve on national guideline committees for establishing standards of care for HDR prostate brachytherapy, visitors from around the world come and train at UCLA to learn this technique, and members of the Division are invited to speak/teach nationally and internationally on HDR prostate brachytherapy.
We are also one of the few Radiation Oncology Departments with a dedicated Brachytherapy Division which includes a brachytherapy procedure suite within the Department as well as an entire team dedicated solely to brachytherapy (Fellow, Physician assistant, Nurse, Dosimetrist, Physicist, Therapist, Scrub tech, and Front desk staff).
References:
- Demanes DJ, Rodriguez RR, Schour L, Brandt D, Altieri G. Int J Radiat Oncol Biol Phys. 2005 Apr 1;61(5):1306-16.
- Hauswald H, Kamrava MR, Fallon JM, Wang PC, Park SJ, Van T, Borja L, Steinberg ML, Demanes DJ. Int J Radiat Oncol Biol Phys. 2015 Aug 5
Who qualifies for HDR prostate brachytherapy and how many treatments is it?
*Candidates for HDR monotherapy
- Low risk (T1, PSA < 10, GS 6)
- Intermediate risk (T1-T2, PSA 10-20, GS 6-7)
- Select favorable high risk (T1-T2), PSA < 20, GS 8)
Length of treatment:
- 2 implants, 1-2 weeks apart, each implant delivers one treatment, 13.5 Gy x 2 (no overnight stay) or
- 1 implant, 10.5 Gy x 3 (overnight stay)
*Candidates for HDR focal monotherapy
- Patients with a local prostate recurrence after having received previous radiation
- Length of treatment: 2 implants, 1-2 weeks apart, each implant delivers 2 treatments, 8 Gy x 4
*Candidates for HDR combination therapy
- Unfavorable high risk patients (T3, PSA > 20, GS 8-10)
- Length of treatment: 1 implant, 1-2 treatments, 15 Gy x 1 or 10.5 Gy x 2 (1 or 2 treatments depends on the size of the prostate gland)
*Whether HDR monotherapy or combination therapy is recommended is ultimately based on numerous factors that will be discussed at the time of consultation. The above are however some general guidelines.
Who qualifies for HDR prostate brachytherapy focal therapy?
Patients who have a local only recurrence after previous radiation therapy are potentially candidates for "focal salvage". In this type of treatment only the area of recurrence is treated rather than retreating the entire prostate gland. The rationale for this is that the majority of men who develop a local recurrence after radiation do so at the site of where the most dominant focus of disease was at the beginning of treatment. The goal of focal salvage is to cure the patient of his disease while limiting the risk of both short and long term side effects. Focal therapy in the up-front setting with no previous treatment is not currently standard of care and is best pursued on a clinical trial.

Above is another example of a focal salvage case of a patient who had a local failure within a cold spot of a LDR seed implant. Again only a portion of the gland was treated for this patient.
HDR brachytherapy procedure
The physician determines whether HDR monotherapy or combination therapy is appropriate for the patient during his initial consultation.
- The usual time between consultation and the first implant is 3-4 weeks.
- For patients who will be receiving HDR combination therapy the brachytherapy is typically done first and the external beam is usually started within 2-3 weeks after completing the brachytherapy. For men who will be receiving androgen deprivation therapy (ADT) they most commonly will be on ADT for two months prior to having their brachytherapy implant.
- Patients need to have some pre-implant lab tests performed as well as a chest X-ray and EKG. Additional testing will depend on the patient’s age and prior medical conditions.
- On the day of the actual procedure the patient is taken to the operating room and given spinal anesthesia (numbs the patient from the waist down) as well as some sedation.
- The patient's legs are place in stirrups and the pelvis is positioned by the physician to access the perineum (the space between the scrotum and anus).
- The physician then uses a template to help direct the treatment tubes called "flexiguides" in and around the prostate. This template has pre-drilled holes arranged in two concentric circles. This circular distribution conforms better to the natural shape of the prostate. The template is held in one hand, while the flexiguides are inserted with the other. Holding the template, rather than having it clamped to the table as in the fixed template technique, allows the physician to tip and angle the template, resulting in more control over where they can place the flexiguides. This is a major advantage as it allows the physician to flare the flexiguides to encompass larger prostates, extracapsular extension, or seminal vesicle involvement.
Below is an example of the standard template that we use for prostate brachytherapy here at UCLA.

Once the flexiguides are in position the template is sutured to the perineum to stabilize the implant.
A camera is used to look into the bladder to ensure appropriate placement of the flexiguides and then a foley catheter is left in the bladder.
After a brief stay in the recovery room the patient has a CT simulation where the placement of the flexiguides is confirmed. Once the images of the implant are obtained the patient waits for the customized treatment plan to be generated.
After the physician approves the treatment plan the patient is moved to the HDR treatment room where the protruding ends of the flexiguides are connected to transfer tubes, which in turn are connected to the HDR machine. Although the patient is alone in the treatment room, he is constantly monitored via a camera and intercom. The patient will hear the afterloader click and a motor running as the radiation source is directed into each of the flexiguides. The Iridium-192 source delivers the radiation dose in about 15 minutes. After the treatment, the source withdraws into the HDR machine. The patient at this point does not have any radiation precautions.
For patients with no overnight stay the implant and the foley catheter will be removed and the patient will go home on the same day after making sure the patient can urinate on his own. For patients with an overnight stay they will spend the night in the outpatient surgery center. The next morning, the second treatment is given. This second treatment requires much less time because the simulation and treatment planning process does not need to be done again. Just a pre-treatment CT scan is performed to verify that the implant hasn't moved overnight and then the patient is treated. After the final treatment the implant and foley catheter are removed and we make sure the patient can urinate on his own.
For patients who are going to have a second implant this is usually done 1-2 weeks later following the same procedure as described above.
HDR prostate brachytherapy treatment planning
One of the great advantages of HDR over permanent seeds is the ability to evaluate the implant in 3-dimmensions and to know what the doses are going to be before any treatment is given. The ability to control the time the HDR radiation source spends in each dwell position allows for much greater target conformity and normal tissue sparing.

One way of evaluating the quality of an implant is to plot a dose volume histogram (DVH). A DVH tells the physician how much of the target volume is covered by the 100% prescription dose, and how much of the prescription dose the rectum and urethra receive. At UCLA, we routinely see 95% or higher, coverage to the target volume, which includes the proximal seminal vesicles and a margin around the prostate to include any extracapsular extension. The actual prostate receives 10% to 25% higher than the prescription dose. This results in a D90 (the dose 90% of the prostate volume receives) of 105 to 113% compared to most permanent seed implants which are considered ‘optimal’ if the D90 is 90%. In a recent publication looking at the consistency of HDR prostate implants performed by our group we observed that the 93% of the D90 values were between 105-115% (1). This demonstrates that our technique allows us to consistently achieve complete prostate target coverage.

HDR Dose Distribution
This is a transverse view of a typical prostate implant showing the radiation "isodose" levels. The blue dots are the superimposed dwell positions along the 17 catheters. (imagine looking end on at a string of beads).
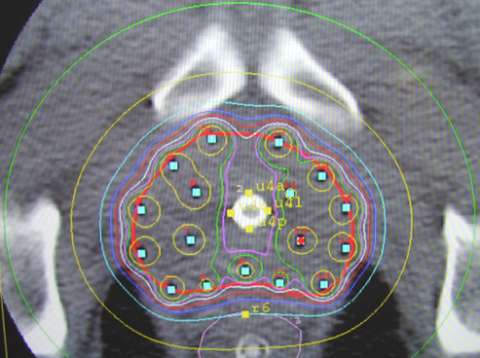
Notice the central area of reduced dose created by the ability to adjust the time the source spends in the 5 interior catheters to spare the urethra (outlined with yellow dots). Also notice the space between the implant and the rectal points. In its natural position, the prostate lies on top of the anterior rectum, separated by a thin layer of tissue, called fascia. The non-fixed template technique allows the physician to slightly lift the prostate away from the rectum, reducing rectal dose. The HDR system allows for dose adjustments and the treatment is delivered in minutes while the rectum is empty. These advantages over permanent seeding are the reasons why the leading centers that perform HDR implants are all reporting very low, if any, rectal complications. Permanent seeds can shift from their original ideal positions resulting in the actual dose distribution not being like the approved pre-plan. With the HDR system, the prostate is held in position by the catheters and the catheters are held in position by the template. If the patient moves, the implant moves with him. HDR is the most accurate method of radiation dose delivery available.
Customizing the Dose Distribution
If necessary, we can create an even larger margin simply by increasing the dwell times, while maintaining the lower doses to the nearby structures and urethra. This ensures that any extracapsular extension (ECE) is adequately treated. The radiation from permanent seeds cannot reach much more than 2 to 3 mm outside the prostate capsule. Knowing this, some seed physicians try to treat ECE by placing permanent seeds in the loose, connective tissue around the prostate. If seeds shift within and migrate out of the firmer tissue of the prostate, it is questionable as to where seeds intentionally placed outside the prostate end up and the coverage and accuracy of the dose supposedly delivered to treat ECE.
We also have the ability to deliver either focal treatments to just part of the prostate gland either as the sole treatment or as a boost to just a specific area within the prostate. We are most commonly using focal treatment in the “salvage” setting at this time.
Some patients have a history of a transurethral resection of the prostate (TURP). This is a common procedure done to relieve pressure of an enlarged prostate on the urethra. An incision is made in the urethra and part of the urethra and prostate tissue is removed. Some men experience some incontinence after this procedure. In order to avoid exacerbating this situation, we spare the TURP defect as much as possible by limiting the radiation dose to less than 105% of the prescription dose. We have found that this dose is tolerated by the urethra while still delivering the necessary tumoricidal dose to the prostate. The HDR system allows for much greater conformality than permanent seeds. With seeds, one hopes that they don’t move near or into the defect and the dose to the defect is not known after the one month post-implant dosimetry is done. With HDR, we can accurately shape the radiation dose to avoid the defect while knowing what the doses will be before any treatment is given.

HDR Conformity and Accuracy Sparing a TURP defect: The image to the right shows how we can accurately shape the radiation dose (white line) to go around the contrast-filled TURP defect. This precision is not possible with EBRT or permanent seeds.
References:
White EC, Kamrava MR, Demarco J, Park SJ, Wang PC, Kayode O, Steinberg ML, Demanes DJ. Int J Radiat Oncol Biol Phys. 2013 Feb 1;85(2):543-8.
Results of HDR prostate brachytherapy at UCLA
Many groups are now publishing their excellent results using both HDR monotherapy and HDR combination therapy. We have been following our patients treated with HDR since the 1990’s and have reported our outcomes with both HDR monotherapy (one of the largest and longest follow-up experiences in the literature to date) as well as HDR combination therapy.
HDR Monotherapy
Outcomes on 448 men (288 low risk and 160 intermediate risk) with prostate cancer treated between 1996-2009 with HDR monotherapy was recently reported in the International Journal of Radiation Oncology Biology and Physics in 2015. With a median follow-up period of 6.5 years the 10 year PSA progression free survival using the Phoenix definition was 97.8%. There were no late serious (Grade 3 to 4) rectal toxicities and 5% rate of urinary toxicities (1).
HDR Combination therapy
Outcomes on 209 men with prostate cancer treated between 1991-1998 with HDR combination therapy was also reported in the International Journal of Radiation Oncology Biology and Physics in 2005. With a median follow-up of 7.25 years the 10 year PSA progression free survival using the Phoenix definition for low, intermediate, and high risk patients was: 93%, 82%, and 62%. There were no serious late (Grade 3 to 4) rectal toxicities and 7.7% urinary toxicities (2).
Since the time of this publication in 2005 we have delivered a higher boost dose which has improved PSA control outcomes and have moved towards CT based planning which has reduced the risk of both short and long term complications to the bladder and rectum.
References:
- Hauswald H, Kamrava MR, Fallon JM, Wang PC, Park SJ, Van T, Borja L, Steinberg ML, Demanes DJ. Int J Radiat Oncol Biol Phys. 2015 Aug 5
- Demanes DJ, Rodriguez RR, Schour L, Brandt D, Altieri G. Int J Radiat Oncol Biol Phys. 2005 Apr 1;61(5):1306-16.
Side effects of HDR prostate brachytherapy
The possible post-HDR acute side effects, usually lasting two to four weeks, are urgent urination, frequent urination and decreased urinary stream. There may also be some transiently more frequent bowel movements or urgency with bowel movements. The perineal area will be tender for a few days so activities like bicycle riding that put pressure on this area should be avoided. Medications are prescribed to help alleviate these temporary side effects. In the long term our most recent HDR monotherapy experience demonstrates very low rates of serious either rectal or urinary side effects. In the long term there is also a risk of developing erectile dysfunction.
Follow-up care after HDR prostate brachytherapy
Patients are usually seen in follow-up within 1-2 weeks of their last implant.
Patients will then have their PSA checked every 6 months for the first 5 years and then annually thereafter.
Information for patients preparing for prostate brachytherapy
UCLA publications on prostate brachytherapy
Laviana AA, Ilg AM, Veruttipong D, Tan HJ, Burke MA, Niedzwiecki DR, Kupelian PA, King CR, Steinberg ML, Kundavaram CR, Kamrava M, Kaplan AL, Moriarity AK, Hsu W, Margolis DJ, Hu JC, Saigal CS. Cancer. 2015 Nov 2.- Hauswald H, Kamrava MR, Fallon JM, Wang PC, Park SJ, Van T, Borja L, Steinberg ML, Demanes DJ. Int J Radiat Oncol Biol Phys. 2015 Aug 5
Banerjee R, Park SJ, Anderson E, Demanes DJ, Wang J, Kamrava M.
Brachytherapy. 2015 May-Jun;14(3):366-72.
Mesko S, Park SJ, Kishan AU, Demanes DJ, Kamrava M.
Brachytherapy. 2015 Mar-Apr;14(2):173-8.
Demanes DJ, Ghilezan MI.
Brachytherapy. 2014 Nov-Dec;13(6):529-41.
Anderson ES, Margolis DJ, Mesko S, Banerjee R, Wang PC, Demanes DJ, Kupelian P, Kamrava M. Brachytherapy. 2014 May-Jun;13(3):292-8.
Mesko S, Kupelian P, Demanes DJ, Huang J, Wang PC, Kamrava M.
Prostate Cancer. 2013;2013:717080.
Kamrava M, Rwigema JC, Chung M, Banerjee R, Wang J, Steinberg M, Demanes DJ.
J Contemp Brachytherapy. 2013 Sep;5(3):127-33.
Kamrava M, Chung MP, Kayode O, Wang J, Marks L, Kupelian P, Steinberg M, Park SJ, Demanes DJ. Brachytherapy. 2013 Sep-Oct;12(5):434-41.
White EC, Kamrava MR, Demarco J, Park SJ, Wang PC, Kayode O, Steinberg ML, Demanes DJ. Int J Radiat Oncol Biol Phys. 2013 Feb 1;85(2):543-8.
Buyyounouski MK, Davis BJ, Prestidge BR, Shanahan TG, Stock RG, Grimm PD, Demanes DJ, Zaider M, Horwitz EM. Brachytherapy. 2012 Jul-Aug;11(4):299-305.
Yamada Y, Rogers L, Demanes DJ, Morton G, Prestidge BR, Pouliot J, Cohen GN, Zaider M, Ghilezan M, Hsu IC; American Brachytherapy Society.
Brachytherapy. 2012 Jan-Feb;11(1):20-32.
Nag S, Demanes DJ, Hagan M, Rivard MJ, Thomadsen BR, Welsh JS, Williamson JF.
Pract Radiat Oncol. 2011 Oct;1(4):218-223.
Demanes DJ, Martinez AA, Ghilezan M, Hill DR, Schour L, Brandt D, Gustafson G.
Int J Radiat Oncol Biol Phys. 2011 Dec 1;81(5):1286-92.
Erickson BA, Demanes DJ, Ibbott GS, Hayes JK, Hsu IC, Morris DE, Rabinovitch RA, Tward JD, Rosenthal SA. Int J Radiat Oncol Biol Phys. 2011 Mar 1;79(3):641-9.
Rosenthal SA, Bittner NH, Beyer DC, Demanes DJ, Goldsmith BJ, Horwitz EM, Ibbott GS, Lee WR, Nag S, Suh WW, Potters L; American Society for Radiation Oncology; American College of Radiology. Int J Radiat Oncol Biol Phys. 2011 Feb 1;79(2):335-41.
Demanes DJ, Brandt D, Schour L, Hill DR.
Am J Clin Oncol. 2009 Aug;32(4):342-7.
D’Ambrosio DJ, Pollack A, Harris EE, Price RA Jr, Verhey LJ, Roach M 3rd, Demanes DJ, Steinberg ML, Potters L, Wallner PE, Konski A. Int J Radiat Oncol Biol Phys. 2008 Mar 1;70(3):671-7.
Martinez AA, Demanes DJ, Galalae R, Vargas C, Bertermann H, Rodriguez R, Gustafson G, Altieri G, Gonzalez J. Int J Radiat Oncol Biol Phys. 2005 Aug 1;62(5):1322-31.
Demanes DJ, Rodriguez RR, Schour L, Brandt D, Altieri G. Int J Radiat Oncol Biol Phys. 2005 Apr 1;61(5):1306-16.
Devlin PM, Brus CR, Kazakin J, Mitchell RB, Demanes DJ, Edmundson G, Gribble M, Gustafson GS, Kelly DA, Linares LA, Martinez AA, Mate TP, Nag S, Perez CA, Rao JG, Rodriguez RR, Shasha D, Tripuraneni P. Int J Radiat Oncol Biol Phys. 2002 May 1;53(1):104-15.
Demanes DJ, Rodriguez RR, Altieri GA.
Radiother Oncol. 2000 Dec;57(3):289-96.
Rodriguez RR, Demanes DJ, Altieri GA.
Hematol Oncol Clin North Am. 1999 Jun;13(3):503-23.