Chair's Message Archive - 2022
December 2022
New Curriculum Updates
Starting in July 2022, our residency program has implemented an updated curriculum. The changes were based on recommendations from a 2-phase residency program review performed by 2 committees composed of faculty and a resident representative. The main goals of the curriculum review are to:
- Encourage trainees to appropriately personalize their training with ample elective opportunities coupled with mentoring from Education leadership and faculty mentors
- Provide progressive learning with graduated responsibility (including senior resident rotations that involve direct supervision of junior residents and preliminary sign out responsibilities for qualified senior residents)
- Leverage educational themes (such as with thematically related rotations in progression)
- Increase the frequency of trainee exposure to subspecialty areas (to provide experiences on rotations as both a junior and senior resident)
The review committees stressed important changes to ensure resident education meets the needs of today’s pathologists and pathology trainees. Some key curricular updates included:
- Shifting to 2 week AP service rotation blocks, to ensure early exposure to all AP subspecialties well in advance of fellowship application deadlines
- Vacation blocks paired with mini-electives
- Dedicated rotations in dermatopathology and neuropathology, rather than pairing these with other services
- New recommendation for an elective pediatric pathology rotation at CHLA
- Decreased autopsy service requirements
- Overall increase in elective time to provide immense flexibility to meet the varied career goals of our diverse residency class
it is anticipated that the increased elective time will provide new opportunities for graduated responsibility and near independent practice experiences. Additionally, the curriculum has been restructured to ensure residents rotate on most AP and CP services at least once per year in PGY1-3 to ensure early broad exposure prior to fellowship selection, minimize large gaps between subspecialty educational experiences, and increase chances for leveraging this early broad exposure to accelerate overall learning.
TRAINEE HIGHLIGHTS

CAP Resident Forum - We thank (from left to right) Drs. Amanda Zand (PGY-2), Danny Rodriguez (PGY-4), Rak Tyagi (PGY-2) and Chana Sachs (PGY-4) for representing UCLA!

Precious Fortes, MD (PGY-3) presented a poster abstract at the annual College of American Pathologist (CAP) conference in New Orleans, LA on an interesting case of intravascular large B-cell lymphoma (IVLBCL) mimicking an allergic/hypersensitivity reaction.

Dr. Irene Riahi, MD (PGY-3) (on right, pictured with Dr. Bita Naini) - CAP22 poster presentation. Case report of a young woman with persistent elevated liver enzymes since her first pregnancy, initially diagnosed as an autoimmune hepatitis/primary biliary cholangitis (AIH/PBC) overlap syndrome, despite negative autoimmune serologic studies, and with no response to steroid treatment. Further investigation and molecular testing at UCLA revealed a heterozygous mutation in the ABCB4 gene. This case highlights the importance of clinicopathologic correlation and that MDR3 deficiency needs to be included as a diagnostic consideration in cholestatic liver diseases of not only infants but also adults. ABCB4 gene mutation analysis will help establish the diagnosis and avoid unnecessary treatment.
Contributors: Dr. Yipeng Geng and Dr. Bita Naini

Precious Fortes, MD (PGY-3) also presented a virtual abstract at the annual AABB 2022 meeting this year with Dr. Dawn Ward, Aaliyah N Pritchett (UCLA undergraduate student), Thomas L King (UCLA Blood and Platelet Center), Dr. Zhen Wei Mei, Dr. Andrea M. McGonigle and Dr. Alyssa Ziman on an EDI focused project: Diversifying the Blood Supply: Addressing Barriers through a Collaborative Black History Month Celebration Blood Drive.

ASDP Meeting in Chicago - We are delighted (from left to right) Drs. Josh Pierce (PGY-2), Sophia Thorne (Dermpath Fellow) and Joe Giessinger (PGY-1) were able to attend!

Precious Fortes, MD (PGY-3) (on right, pictured from left to right with Drs. Theresa Kim (Cytopathology Fellow) and Erika Rodriguez) recently co-presented two projects at the International Congress of Cytology and American Society of Cytopathology annual meeting in Baltimore, MD. She presented a comprehensive study of thyroid fine needle aspiration in pediatric and young adult patients at UCLA and co-presented the effect of touch preparations on tissue adequacy for ancillary testing of transthoracic core needle biopsies with Dr. Teresa Kim (UCLA Cytopathology Fellow). Her project mentors, Dr. Erika F. Rodriguez and Dr. Jeffrey Krane also attended and presented.

Amanda Zand, MD (PGY-2) (on left, with Dr. Erika Rodriguez) presented a QA project at the American Society of Cytopathology annual meeting. It compared the turnover time and accuracy rates for pancreas FNA and core needle biopsies between the Westwood and Santa Monica Hospital. This included specifically examining splitting vs. lumping of the cytology and surgical pathology cases.

American Society of Cytopathology 2022 Annual Meeting - Clockwise from bottom left, Drs. Theresa Kim, Amanda Zand, Jeffrey Krane (Cytopathology Fellowship Director), Erika Rodriguez and Precious Fortes.
November 2022
Immunogenetics Updates
I am pleased to share with you some of the many research collaborations currently taking place in our Department. At UCLA, we are fortunate to have a vibrant research culture within the David Geffen School of Medicine and UCLA campus. Our location on the UCLA campus facilitates collaboration with other Departments, Institutes, Centers and Schools, including the UCLA Samueli School of Engineering, the Broad Stem Cell Research Center and numerous basic science departments within the UCLA College of Letters and Sciences, in addition to the collaborations we enjoy with colleagues in other clinical departments within our School of Medicine. Furthermore, many of our researchers are involved in interesting collaborations with faculty from other universities.

Dr. Valerie Arboleda – Collaboration with Dr. Bianca Russell (Medical Genetics). Dr. Arboleda and Dr. Russell work together to establish a translational research pipeline for the study of pathogenic chromatinopaties. Chromatinopaties are rare genetic disorders caused by genes that function to control epigenetic regulation. Together, they have projects exploring the gene-regulation, cell biology and clinical features underlying this class of disorders.
Collaboration with Dr. Noah Zaitlen on Studying Penetrance and Expressivity of rare genetic mutations on clinical phenotypes. Genetic variants that are associated with disease states can have different effects across individuals. Often, genetic background (other genetic variants in the individual) and environment can modulate the effect of the genetic mutations resulting in less severe or even a lack of phenotype in what was previously thought to be a disease-causing mutations. This study uses large scale biobank data from UCLA and UKBiobank to explore factors that can modulate the effect of clinically pathogenic mutations.
Collaboration with Dr. Manish Butte (MIMG/Pediatrics), Dr. Bogdan Pasaniuc (Pathology), Dr. Harold Pimentel (Computational Medicine) and Dr. Omai Garner (Pathology). Coccidioidomycosis is a dimorphic fungus endemic to the southwestern United States and South America. Rare cases result in disseminated infection that result in lifelong morbidity and mortality. Here we study genetic factors that contribute to susceptibility to disseminated Coccidiomycosis infection.
Collaboration with Dr. Hanna Mikkola (Molecular, Cellular and Developmental Biology), Dr. Keriann Backus (Biological Chemistry) and Dr. Vivian Chang (Pediatric Heme-On) on a research project identifying mechanisms underlying treatment resistance in MECOM rearranged Leukemia stem cells. This project explores how a rare inversion of chromosome 3 results in aberrant expression of MECOM, and oncogenic transcription factor.

Dr. Gay Crooks – Dr. Gay Crooks has initiated a new collaboration with Dr. Donald Kohn (Pediatrics and MIMG) to develop novel base editing therapy for a lethal form of severe combined immune deficiency caused by a mutation in the CD3D gene. Dr. Gloria Yiu (Clinical Instructor in DOM, Division of Rheumatology) is leading the collaboration for the Crooks lab and Grace McCauley leads the Kohn collaboration.

Dr. David Dawson – David Dawson is a physician-scientist who oversees a basic and translational research program in pancreatic cancer. He runs the pancreas biobanking program at UCLA and co-leads the biobanking working group of the University of California Pancreas Cancer Consortium. For over two decades, he has served as a key collaborator or co-investigator on numerous published studies and funded projects focused on pancreatic cancer and related diseases. He actively collaborates with multiple pancreatic disease-focused clinicians and researchers in multiple departments here UCLA, as well as numerous pancreas research investigators from various institutions across the country.

Dr. Wayne Grody
- UCLA Promise Armenian Institute: Armenian Genome Project
- Institute for Precision Health/California Center for Rare Diseases: Familial Mediterranean Fever Biobank and Patient Registry
- Division of Digestive Diseases, Dept. of Medicine: Co-Director, Familial Mediterranean Fever Clinic
- Division of Medical Genetics, Department of Pediatrics: Attending Physician and research collaborator, Clinical Genetics
- School of Dentistry: Several NIH-funded Projects on Saliva-omics for Early Detection of Cancer
- Lundquist Institute, Harbor-UCLA: Polygenic Risk Scores in the Armenian Population
- Department of Human Genetics: UCLA Clinical Site for Investigation of Undiagnosed Disorders
- Division of Ambulatory Pediatrics, Department of Pediatrics: Genetic Variants in Alstrom Syndrome

Neuropathology + Dr. Harry Vinters – Neuropathology is a collaborative research endeavor. They work on numerous projects with a large variety of investigators in both Clinical & Basic Science Departments. Many of Dr. Vinters' recent papers are co-authored with Dr. Shino Magaki.
- Neurosurgery – Epilepsy Surgery Program. Dr. Gary W. Mathern (50+ co-authored publications), Aria Fallah (5 publications), Carlos Cepeda (many publications), Geoff Owens (several publications)
- Radiology/Radiological Sciences – Multiple projects related to stroke and epilepsy; Dr. Noriko Salamon (34+ publications)
- Neurology – NeuroAIDS research---Dr. Elyse J.Singer (8 co-authored pubs)
- Molecular Biology – Protein structural abnormalities in neurodegenerative diseases—Dr. David Eisenberg (4 publications, including a recent co-authored paper in Nature Communications)
- Neurobiology – Y. Zhang, Michael Sofroniew (a review article I co-authored with Dr. Sofroniew in 2010 just passed 3000 WOS citations)

Dr. Dinesh Rao – Dinesh Rao, MD, PhD is leading a major project on developing small molecule inhibitors of RNA binding proteins. For this project he is collaborating with Dr. Neil Garg, Professor and Chair of Chemistry and Biochemistry and Dr. Robert Damoiseaux, Professor of Medical and Molecular Pharmacology and Director of Molecular Screening Shared Resource. The interdepartmental collaboration is expected to yield new small molecular probes and potential cancer therapeutics and is funded by the UCLA innovation fund and the California Institute of regenerative Medicine.

Dr. Peter Tontonoz – The Tontonoz laboratory has an ongoing collaboration with Dr. Mike Jung’s group in the department of Chemistry. This joint effort aims to synthesize and characterize novel small molecules inhibitors of cholesterol transport.

Dr. Lily Zhang – Dr. Zhang has been collaborating with Dr. David Wong at School of Dentistry. They recently submitted a new NIH grant proposal entitled “Multi-Omics cfDNA Biomarkers for Liquid Biopsy Early Detection of Gastric Cancer”.
Dr. Zhang started a new collaboration with GYN oncologist Dr. Gottfried Konecny on “Early detection of ovarian cancer using cfDNA”.

Dr. Yazhen Zhu – To facilitate translational research on liquid biopsy-based cancer and prenatal diagnostic assay development, they established an extensive collaboration network, including i) Dr. Vatche Agopian in UCLA Liver Transplant Program on developing circulating tumor cells (CTC) and extra-cellular vesicles (EV)-based diagnostic and prognostic assays in hepatocellular carcinoma (HCC), ii) Dr. James Wu in UCLA Surgery on developing CTC/EV-based digital scoring system to avoid unnecessary diagnostic surgery and overtreatment in thyroid nodules, iii) Dr. Wanxing Chai-Ho in UCLA Oncology on developing CTC-based HPV E6/E7 digital scoring assay to better predict the prognosis of HPV-positive oropharyngeal carcinoma, iv) Dr. Yalda Afshar in UCLA Obstetrics on developing circulating trophoblast (cTB)-based diagnostic assays for early detection of placenta accrete spectrum.
UIC Collaborations

Dr. Michelle Hickey – Funded subcontract with Baylor/Texas Children’s Hospital to study non-HLA antibodies in pediatric heart transplant patients

Dr. Elaine F. Reed
- Drs. Elaine Reed, Joanna Schaenman (Department of Medicine, UCLA), Michael Yeaman (Lundquist Institute), and Loren Miller (Lundquist Institute) are collaborating with Dr. Arleen Brown (UCLA) and Dr. Keith Norris (UCLA) on a study to advance mutual goals and synergistic opportunities for CEAL / STOP COVID-19 and LA-SPARTA with a focus on at-risk and underserved populations disproportionately impacted by this pandemic. A translational purpose of this initiative is to enhance personal and public health education about SARS-CoV-2 to promote improved outcomes in underserved persons at highest risks of exposure and greatest vaccine hesitancy.
- Dr. Elaine Reed is collaborating with Dr. Mario Deng, Department of Medicine and Director of the Advanced Heart Failure Program, Division of Cardiology on a NIAID funded grant to study multi-dimensional outcome prediction algorithm for hospitalized COVID-19 patients. The major goal of the research is to study Severe acute respiratory syndrome coronavirus 2 (SARSCoV-2)-mediated coronavirus disease (COVID-19) is an evolutionarily unprecedented natural experiment that causes major changes to the host immune system.
- Dr. Elaine Reed is collaborating with Dr. David Briscoe from Boston Children’s Hospital on a NIAID funded grant to study advancing transplantation outcomes in children. The major goal of this research is to characterize HLA DSA and non-HLA antibody prevalence, strength/titer, subclass and functional characteristics in pediatric patients treated with belatacept and mTORi based maintenance immunosuppression with depletional induction.
- Dr. Elaine Reed is collaborating with Dr. Joren Madsen, Harvard University on a NIAID funded grant to study targeting inflammation and alloimmunity in heart transplant recipients with tocilizumab. The major goal of this research is to compare efficacy of standard triple maintenance immunosuppression plus TCZ treatment versus standard triple maintenance immunosuppression plus placebo (saline) on heart transplant outcome.
- Dr. Elaine Reed and Dr. Ting Ting Wu (UCLA) are collaborating with Dr. Ted Ross from the University of Georgia on the NIAID funded CIVICs grant to develop more effective vaccines for influenza.
- Dr. Elaine Reed is collaborating with Dr. John Belperio, Department of Pulmonology, Lung Transplant Surgery on a NIAID funded grant to study clinical trials in organ transplantation in children and adults (CTOT-CA). The major goal of this research is to determine if Itacitinib increases lung transplant recipient’s infectious risks (allograft and systemic infections, bacterial, viral, fungal, atypical mycobacteria) and importantly if Itacitinib alters the allografts inflammatory milieu that protects the allograft from the convergence to CLAD post infection.
- Dr. Elaine Reed is collaborating with Dr. Jerzy Kupiec-Weglinski, Department of Surgery and Director of the Dumont-UCLA Transplantation Research Laboratories in the Division of Liver and Pancreas Transplantation on a NIAID funded grant to study innate-adaptive immunoregulation in liver transplant ischemia/reperfusion injury. The major goal of this research is to better understand the interplay between innate and adaptive immune systems in IRI from human liver transplant recipients.

Dr. Rebecca Sosa
- Elaine Reed and Rebecca Sosa collaborated with several UCLA departments on a project, which was published in :
- Department of Pathology and Laboratory Medicine
- UCLA Immunogenetics Center
- OneLegacy
- Department of Microbiology, Immunology and Molecular Genetics
- Department of Pediatrics
- Department of Molecular and Medical Pharmacology
- LifeStream Blood Bank
- Department of Surgery
- Department of Medicine
- Department of Urology
- They investigated the use of apheresis to collect mobilized peripheral blood hematopoietic stem cells (HSCs) for transplant tolerance. They determined that HSCs can be mobilized and collected from the peripheral blood of brain-dead donors without sacrificing the transplant ability of deceased donor livers. This is an important first step toward immunosuppression-free deceased donor transplantation.

Dr. Nicole Valenzuela – A collaboration between the laboratories of Nicole Valenzuela (UCLA Pathology and Laboratory Medicine), Matteo Pellegrini (UCLA Molecular, Cell and Developmental Biology), and Patrick Murphy (UConn Health) is using cutting-edge single nucleus multi-omics to profile the endothelial cell transcriptomic and nuclear proteomic signatures of clinical heart transplant rejection. This project capitalizes on the UCLA Department of Pathology and Laboratory Medicine’s bioarchive of remnant heart transplant biopsies, and aims to provide needed insights into the vascular molecular phenotypes of alloimmune injury to identify novel therapeutic targets for this disease.
October 2022
Immunogenetics Updates
CLINICAL
- Article “HLA Antibody Identification by Luminex Single Antigen Bead Assay – Intralaboratory Comparison” by Arlene F. Locke, B.S. was highlighted in the ASHI Quarterly newsletter under the Technologist Innovations and Insights section.
- Anh Du and John Muramoto have both been promoted to CLS Supervisors for the Immunogenetics Center. They will both oversee the molecular and clinical areas of the lab.
- The UIC welcomes our new personnel to the team!
- Rosa Osegueda, HLT
- Angela Fronda, HLT
- Bernard Baylosis, HLT
- Michael Nossair, CLS
- Wael Ishaq, CLS
- Kathleen Noche, CLS
- Marvin Salazar, CLS
- Juan Tao, CLS
- Zahra Faghiri, CLS
- Hannah Ochoa Sanchez, SRA
- Itzel Ramirez, SRA
QUALITY IMPROVEMENT
- The UCLA Immunogenetics Center is committed to continuous quality assessment and improvement. Quality Improvement projects are in alignment with the Department, Health System and Faculty Practice Group strategic goals for patient care/safety, and operational excellence.
- Highlighted is our most recent project:
- Improving Discrete Reporting of Clinical/Diagnostic Data for Transplant Patients
- Problem: Quality Assessment of clinical/diagnostic data to assess for transplant patient outcomes requires significant, time-consuming manual data collection.
- Solutions: (1) Develop natural language processing that will identify critical data elements from textual interpretative comments in biopsy and antibody reports; (2) Develop IT interventions to guide ordering of tests and biopsy at time of suspected rejection; (3) Develop an electronic visual analytics dashboard for faster Quality Assessment of clinical-diagnostic data to assess for rejections and appropriateness of treatment and clinical care.
- Improving Discrete Reporting of Clinical/Diagnostic Data for Transplant Patients
EDUCATION
- UIC welcomes our new fellow for 2022-2024, Dr. Nezar Eltayeb-Elsheikh, Ph.D., to our team.
PUBLICATIONS/ABSTRACTS/AWARDS
- UIC faculty and fellows published 13 publications and numerous abstracts presented at national society conferences.

Dr. Nicole Valenzuela was awarded the 2022 American Society of Transplantation, Distinguished Early Career Award.

Dr. Elaine F. Reed was awarded the 2022 Outstanding Achievement in Transplantation Science (Mentorship or Education & Training) Award by The Transplantation Society.
Laboratory Medicine Updates
The Clinical Chemistry section, under the leadership of Dr. Lu Song, section chief, and Dr. Imir Metushi, has been extremely busy maintaining high quality patient testing while making significant progress on several initiatives to ensure that our laboratories provide innovative high-quality patient testing to meet the health system’s needs.
Our clinical laboratories are implementing total laboratory automation (TLA) at all three sites (Ronald Reagan Core Laboratory (RR), Santa Monica Core Laboratory (SM) and BURL Outreach Clinical Laboratory). This automation will allow all three sites to process patient specimens more efficiently, seamlessly accommodate add-on test requests, and decrease turn-around-times, thereby improving patient care. BURL was the first laboratory to go live with TLA in July 2022 which included the addition of the Roche pre-analytic P612 module into the line where samples are received, aliquoted and directed for testing to the Cobas chemistry or immunoassay units. The next step for BURL is to optimize workflow of the current TLA system to increase efficiency so that we can add HbA1c and hematology testing to the TLA line. SM is currently in the early phase of TLA implementation working on installation and validation.
Simultaneously, our clinical chemistry section has made significant updates to several tests to serve patients better. eGFR and high sensitivity troponin are two significant examples of these updates. Drs. Song and Metushi collaborated with nephrology and IT departments to successfully switch the eGFR calculations using the 2021 CKD-EPI equations without race variables on June 1, 2022. We also validated the eGFR calculation using whole blood creatinine measured with blood gas analyzers so that patients in the emergency department and nuclear medicine can receive eGFR results in a timely manner when their creatinine is measured in whole blood near point of care. On September 21, 2022, our laboratories started offering a testosterone profile which includes free and bioavailable testosterone. By performing this profile in-house, our laboratory can provide a shorter turnaround time when compared to testing performed at a reference laboratory, and thus better meet the needs of our patients and clinicians. Our team is currently working on the implementation of a high-sensitivity troponin assay (hsTnl), the latest generation of the cardiac enzyme testing that allows for detection of very low levels of troponin T, helping to diagnose heart attacks more quickly. To date, RR and SM labs have completed the technical validation of hsTnI tests on the Beckman Access 2. Next steps involve working with cardiologists to develop educational materials for all clinicians within UCLA health system.
We are grateful for Drs. Song and Metushi’s leadership with these projects, and thank our laboratory staff and IT colleagues for their hard work, dedication and partnership!
September 2022
The Pathology EDI committee has been hard at work developing the JEDI Plan (Justice, Equity, Diversity, and Inclusion) and is excited to begin the execution phase to accomplish our FY23 goals. The JEDI Plan outlines overarching department goals over a 3-5 year period for the following domains: People, Climate, Structural Elements, Professional Development/Education, Community Engagement, and Patient Care. The goals will be evaluated each year to discern progress made and identify improvement areas. They will establish subcommittees for each domain, so if you are interested in joining, please be on the lookout for an email that will be sent out shortly from EDI Co-Chairs about their upcoming meeting to review the JEDI Plan in detail. Aside from the JEDI Plan, the EDI committee has accomplished the following action items:
- Successfully completed their first book review of Caste by Isabel Wilkerson and will be ramping up for the second iteration of their book club soon.
- Developed a Grand Rounds demographics survey for the speakers.
- Held the first EDI Grand Rounds of the year on August 12, 2022, with Dr. Joely Straseski from the University of Utah, ARUP Labs: “Inclusive laboratory testing for transgender individuals: focus on utilization and reporting”
- Scheduled two other EDI Grand Rounds for the remainder of the calendar year:
- October 28, 2022: “Racial disparities in cardiovascular medicine; racial differences in cardiovascular complications due to COVID-19 from autopsy studies” - Speakers: Karol Watson, MD, PhD, UCLA DGSOM, and Rick Vander Heide, MD, PhD, Marshfield Clinic, WI
- November 4, 2022: “Removing race from eGFR equation and equity in kidney transplantation” - Speaker: Irene Kim, MD, Cedars-Sinai
Please view the of our Department EDI committee’s purpose, key priorities, and overview of our JEDI Plan. We look forward to advancing our EDI initiatives in the coming year. If you have any questions, concerns, or suggestions, please email the EDI Co-Chairs at .
As a department, we will continue to focus on community engagement and opportunities to advance education, research, and scientific discovery.
August 2022
The Department of Pathology & Laboratory Medicine offers and/or participates in six Allied Health training programs. Depending on the specific program, we offer both independent training at UCLA, or act as a rotation site for practical clinical experiences for students enrolled in degree programs elsewhere. Staff are essential members of our successful health care team, and we are proud to help train the next generation of Lab Scientists, Phlebotomists, Cytologists and Pathologist Assistants! Our allied health students work closely with our staff, residents, fellows and faculty during their time at UCLA Pathology.
We also offer experiences for local high school students and recent high school graduates who participate in the Turner UCLA Allied Health Internship. This Internship exposes students to allied health careers throughout the hospital. For more information and to view program videos, please visit their .
Limited License Clinical Cytogeneticist Scientist Program
The primary goal of this program is to train qualified individuals for eligibility and licensure as Clinical Cytogeneticist Scientists by the state of California. The program provides scientific background, individual training and supervised performance of laboratory tests. Interpretation and troubleshooting skills are emphasized, followed by competency evaluation and documentation. The laboratory experience is supplemented by self-instructional materials.
Limited License Clinical Immunohematology (Blood Banking) Scientist Program
The primary goal of this one year program is to train qualified individuals for eligibility and licensure as Clinical Immunohematology Scientists by the State of California. The program will include both laboratory and didactic training in high complexity testing including ABO/Rh testing, unexpected antibody detection, compatibility testing, antibody identification and routine problem solving, as well as blood donor selection, blood collection and processing, blood component preparation for storage and administration, and the quality control of blood bank equipment and reagents. The laboratory experience and didactic lectures are supplemented by attendance at selected conferences, self-study material and homework assignments.
Limited License Clinical Genetic Molecular Biologist Scientist (CGMBS) Program
The primary goal of this program is to train qualified individuals for eligibility and licensure as Clinical Genetic Molecular Biologist Scientists (CGMBS) by the State of California. The program provides scientific background, individual training and supervised performance of laboratory tests. Interpretation and troubleshooting skills are emphasized, followed by competency evaluation and documentation. The laboratory experience, educational lectures and conferences are supplemented by self-instructional materials, e.g., tapes, slides.
Clinical Laboratory Scientist Program
Clinical laboratory testing plays a crucial role in the detection, diagnosis, and treatment of disease. Clinical Laboratory Scientists (CLS) perform and supervise laboratory testing in the clinical laboratory specialty areas of biochemistry, hematology, medical microbiology, immunohematology, immunology, molecular diagnostics, serology and clinical microscopy. Licensed CLS perform diagnostic testing in hospital clinical laboratories, commercial reference laboratories, or in research and development for biotechnology companies. The post-baccalaureate clinical training program in affiliation with California State University, Dominguez Hills currently accepts eight students per year. Graduates of the program are eligible for the Medical Laboratory Scientist (MLS) certification examination of the American Society of Clinical Pathology (ASCP) Board of Certification (BOC) and for CLS licensure by the California State Department of Health.
Limited License Clinical Microbiologist Scientist Program
The primary goal of this program is to train qualified individuals for eligibility and licensure as Clinical Microbiologist Scientists by the state of California. The program provides scientific background, individual training and supervised performance of laboratory tests. Interpretation and troubleshooting skills are emphasized, followed by competency evaluation and documentation. The laboratory experience, didactic lectures and conferences are supplemented by self-instructional materials, e.g., tapes, slides.
Medical and Public Health Laboratory Microbiology
The UCLA CPEP fellowship experience is designed to provide comprehensive training to well-qualified academically-oriented individuals that will prepare them for careers as directors of clinical microbiology or public health laboratories. The content and extent of training is tailored to each individual entering the program according to their unique background and interests. The training occurs primarily in the UCLA Clinical Microbiology Laboratory. Training in the clinical aspects of infectious disease occurs at the West Los Angeles Veterans' Administration Medical Center and at the Westwood Ronald Reagan UCLA Medical Center.
School of Cytology
The School of Cytology, founded in 1991, is accredited by the Commission on Accreditation of Allied Health Education Programs (CAAHEP), and offers a comprehensive course in Cytology. This one-year training program trains students to detect cancer, its precursors and other medical disorders. Students will learn to perform a variety of diagnostic and research procedures in the Cytology laboratory, including microscopic examination of human cellular material and processing and staining of cytological specimens. The student will be trained to assess adequacy at fine needle aspirations and other procedures. Students will also have opportunities to learn new technologies in Cytology.
For more information, please visit .
Pathologists’ Assistants Program
A pathologists’ assistant is a highly trained, certified allied health professional who is qualified by academic and practical training to provide various services in anatomic pathology under the direction and supervision of a licensed, board-certified, or board-eligible anatomic pathologist. Pathologists’ assistants work in hospitals, pathology labs, forensic labs, and morgues.
Pathologists’ Assistants perform accurate and timely processing of a variety of laboratory specimens, comprehensive macroscopic examinations, evaluating all surgical pathological specimens, and Research and training pathology residents, pathologists’ assistant students, and other pathology lab personnel.
Pathologists’ Assistants also perform postmortem examinations including prosection, assisting the pathologist with rendering the provisional anatomic diagnosis, composing the clinical history, recording the macroscopic anatomic findings, and submitting tissue sections for microscopic examination.
Pathologists’ Assistants play a critical role in the delivery of healthcare services in both surgical and autopsy pathology. They are key partners in assisting the Pathologist to arrive at a pathologic diagnosis, but it is the sole responsibility of the Pathologist to render a diagnosis.
Our staff provides clinical training to second year Pathologists’ Assistant students who have completed their didactic training at a National Accrediting Agency for Clinical Laboratory Sciences (NAACLS) program by exposing them to a variety of laboratory specimens, ranging from simple biopsies to complex resections. During their clinical training, the Pathologists’ Assistant students learn how to evaluate and process all surgical pathological specimens, perform intraoperative specimen analyses (frozen sections), biorepository banking, and autopsies.
Individuals interested in becoming a pathologists’ assistant should take advantage of math and science courses in high school, to prepare for college courses in these subjects. Higher education requirements for a pathologists’ assistant include:
- Bachelor’s degree in one of the life sciences, i.e. biology, chemistry
- Pathologists’ assistant program (a two-year program that results in a master’s degree)
Phlebotomy Technician Program
The primary function of a phlebotomy technician is to obtain patient blood specimens by venipuncture or microtechniques. The phlebotomist aids in the collection and transportation of other laboratory specimens, and may be involved with patient data entry. A phlebotomy technician also draws blood for transfusions, donations and research.
For more information, please visit .
As a department, we will continue to focus on community engagement and opportunities to advance education, research, and scientific discovery.
July 2022
As we begin the new academic year, I would like to provide a warm welcome to our new Residents, Fellows, and Faculty. Additionally, I would like to highlight the Farewell Ceremony awards and recipients.
Please join me in welcoming our new PGY1 Residents!

Erica Fermon
Meharry Medical College

Joseph Giessinger
A.T. Still University of Health Sciences School of Osteopathic Medicine in Arizona

Joel Raqueno
Kansas City University College of Osteopathic Medicine

Yuan Shui
Xiangya School of Medicine, Central South University

Rose Valencia
Western University of Health Sciences College of Osteopathic Medicine of the Pacific

Weibo Yu
Peking Union Medical University
Please join me in welcoming our new
It is with great pleasure I announce our incoming faculty joining the department. Please join me in welcoming Dr. Jennifer Chia, Dr. Jitin Makker, Dr. Dandan Wang, and Dr. Khalda Ibrahim.
Dr. Jennifer Chia will be joining the UCLA Department of Pathology and Laboratory Medicine faculty as a Clinical Instructor, starting July 1, 2022.
Dr. Chia is originally from Boulder, Colorado, where she studied biochemistry at the University of Colorado. She then completed her MD and PhD degrees through the Weill Cornell/Rockefeller/Sloan-Kettering MD/PhD program in New York City, before switching coasts for training in Anatomic Pathology residency and Hematopathology fellowship at UCLA.
Dr. Chia will continue her development as a physician-scientist through the UCLA STAR program postdoctoral track, with interest in hematopoiesis and how dysregulation of the bone marrow microenvironment may contribute to clonal bone marrow disorders. Outside of work, she loves to be outside, and is an avid knitter, reader, and rock climber. We are delighted to welcome Dr. Jennifer Chia in her new role in the section of Hematopathology in the Division of Anatomic Pathology.
Dr. Jitin Makker will be joining the UCLA Department of Pathology and Laboratory Medicine faculty, as an Assistant Professor, starting July 1, 2022.
Dr. Makker is our current fellow in the Combined Clinical Informatics and Surgical Pathology fellowship at the UCLA David Geffen School of Medicine. He is interested in data analytics, digital pathology, and workflow improvement with informatics tools. Dr. Makker obtained his medical degree from India from Sarojini Naidu Medical College, Agra.
He completed his anatomic and clinical pathology residency at University of Southern California. Prior to residency, he did clinical research in gastroenterology and completed a Quality Improvement in Healthcare fellowship at UCLA in the Division of Digestive Diseases. We are delighted to welcome Dr. Jitin Makker in his new role as Clinical Informaticist/Surgical Pathologist in the Division of Anatomic Pathology.
We are pleased to announce that Dr. Dandan Wang will be joining the UCLA Department of Pathology and Laboratory Medicine faculty as a Clinical Instructor, starting July 1, 2022. Dr. Dandan Wang completed her medical training at Sun Yat-sen University of Medical Sciences in Guangzhou, China. Prior to joining UCLA, she did her AP/CP pathology residency training at LAC/USC, followed by a surgical pathology fellowship focused on GI and GU pathology at LAC+USC. She then pursued subspecialty training in Women's Health (gynecology and breast) pathology at UCLA. In her leisure time, she enjoys outdoor activities such as jogging and hiking with family. We are delighted to welcome Dr. Dandan Wang in her new role in the Section of Surgical Pathology in the Division of Anatomic Pathology.
We are pleased to announce that Dr. Khalda Ibrahim will be joining the UCLA Department of Pathology and Laboratory Medicine faculty, as an Assistant Professor, in the Division of Laboratory Medicine starting August 1, 2022. Dr. Ibrahim graduated from the Johns Hopkins University School of Medicine, completed an internship in General Surgery and residency in Anatomic and Clinical Pathology. She joined UCLA two years ago for a combined fellowship in Transfusion Medicine and Clinical Informatics.
Her clinical and research interests include patient safety, machine learning/predictive analytics, and process modeling/workflow analysis. Her work on optimizing transfusion support of patients with sickle cell disease through advanced informatics strategies has received grant funding from UCLA Health, and she looks forward to continuing efforts to advance health equity. She also recently joined the board of Transfusion Antibody Exchange, a non-profit organization that is spearheading efforts to create the first nationwide RBC alloantibody registry in collaboration with blood bank information system vendors, federal agencies, and medical centers.
In her new role, Dr. Ibrahim will initiate and collaborate on laboratory projects utilizing informatics tools to improve the quality of patient care and laboratory operations. She will also have clinical responsibility in the laboratory, and will be actively engaged in resident and fellow education and mentoring with informatics projects. We are delighted to welcome Dr. Khalda Ibrahim in her new role in the Division of Laboratory Medicine.
Please join me in honoring our !
As we start anew, I look forward to our department focusing our continued excellence and advancement in clinical care, education, and research.
June 2022 - Part II
As the academic year comes to a close, I would like to spotlight our graduating trainees, both staff and MD/PhD trainees. We thank them for their dedication and wish them the best in their future endeavors.
Staff and Other Trainees
Clinical Genetic Molecular Biologist Scientist (CGMBS) Program
Nick Samouna

Clinical Laboratory Scientists Trainees, California State University, Dominguez Hills
Patricia Alonzo
Diana Mae Cruz
Carlos Gutierrez
Galen Law
Brent Legaspi
Kathleen Noche
Wilson Pham
Juan Tao

Cytotechs
Adriana Del Barco
Qi Chen
Mindy Pang
Alexa R. Roberts

Clinical Trainees
Please view a our a list of our and their future endeavors.
June 2022 - Part I
The Department of Pathology & Laboratory Medicine is an integral part of the vibrant UCLA research enterprise and includes faculty members with a broad array of basic, translational, and clinical research interests.
Our first annual Research and Clinical Excellence Day was held on Friday, May 20, 2022. The event highlighted the ongoing basic and clinical research in our department. The event included presentations and keynote speakers along with a poster displays. Thank you to our speakers, Drs. Moatamed, Hanlin Wang, Ting Zhang, Jianyu Rao, Jeff Krane and Anica Wandler. Special thank you to Drs. Valerie Arboleda and Bogdan Pasaniuc for their terrific keynote speeches.
The poster presentations were equally diverse. Thank you also to our Department core labs for their talks (Dr. Xinmin Li – TCGB core) and poster presentations (Dr. Clara Magyar – TPCL/PRP and Dr. Monica Cappelletti – IAC).
I’d like to thank Jonathan Said (Vice Chair for Clinical Research) and the Research Day Committee (Drs. Jonathan Said (Chair), Neda Moatamed, Tom Lee, Jasmine Zhou and Bogdan Pasaniuc) for all their work bringing this event into reality.
I am proud to profile our new as of July 1st. We congratulate the faculty principal investigators on their grant awards and look forward to their innovative findings and results.
The above publications, grants and collaborations underscore that UCLA is a highly interactive and collaborative environment in which interdisciplinary research flourishes. Our faculty and students continue to conduct important and meaningful basic, translational and clinical research and I look forward to learning about their future discoveries. Departmental research has continued to thrive and grow over the past decade. Our faculty publish their findings in many of the top biomedical journals such as Cell, Immunity, Molecular Cell, Nature Immunology, and the Proceedings of the National Academy of Sciences. As a small representative snapshot, since March 2021, our faculty has produced over 250 published papers and abstracts. To date for FY22, faculty researchers generated over $2.4 million in active extramural funding, including over $1.9 million from NIH. A comprehensive listing of the department’s Faculty Publications can be found .
May 2022
2021 was a remarkable year for the UCLA Immunogenetics Center (UIC). As we enter 2022, we would like to highlight some of our achievements in clinical, quality, education, research, and areas of innovation.
Clinical
The UCLA Immunogenetics Center (UIC) provided Histocompatibility and Immunogenetics testing for 1,146 solid organ transplants for the 5 transplant centers we serve (UCLA, UC Davis, Harbor-UCLA, Scripps Green Hospital, Saint Joseph’s Orange) and performed Histocompatibility testing for 32 kidney paired donations at UCLA and 166 Bone Marrow Transplant (BMT) for UCLA, UC Davis, and Scripps Green Hospital.
UIC established new partnerships with 5 Regional OPOs & USC, Loma Linda, Cedars Sinai and CHLA to provide crossmatch testing for new UNOS allocation policy.
UIC and the Pathology Business office implemented a new Beaker billing system to increase efficiencies and collections. In addition, they set up a Tableau dashboard for tracking UIC finances and test volumes.
UIC welcomes Krystal Kendall, UIC Laboratory Manager, to our team.
Quality
Major quality projects implemented and completed. Here are highlights of two projects:
- Control samples are an important part of quality control and assurance procedures so that results are reliable. Dr. Monica Cappelletti and Mary Alice Mita set up a consent form for healthy control blood collection mainly in the outpatients setting. The Nurse Supervisors have been instructed on the procedure and a tip sheet has been distributed to the phlebotomist. However, most of the inpatient samples are collected without a control. Thus, the IAC has established a local pool of healthy controls (10 volunteers) to cover all the needs of controls to be run in parallel with the patient’s samples.
- We improved the process of crossmatching transplant patients with living and deceased organ donors. Validation and implementation of the Robosep automated, immunomagnetic, negative cell selection technology resulted in several benefits over the prior manual process including 1) 30% reduction in the time to lymphocyte isolation, 2) 40% reduction in ‘hands on’ technologist time, and 3) 2-3 fold increased efficiency and sample throughput. Using this automated process, unwanted cells in the donor’s blood are bound to magnetic particles, which are then separated from the lymphocytes, eliminating the time-consuming density gradient of the conventional method. The project was led by Project Scientist Dr. Yuxin Yin.
Education
The UIC educational program led by Jennifer Zhang, Ph.D., leveraged the zoom platform to expand training in Immunogenetics and Histocompatibility testing to our partner institutions. The faculty taught 6 educational lecture series to pathology residents, pathology fellows, transfusion medicine fellows, clinicians and transplant coordinators at UCLA, UC Davis, Harbor-UCLA, Scripps Green Hospital, Saint Joseph’s Orange, One Legacy, and Kaiser Permanente Southern California.
Research
UIC faculty and fellows published 24 publications, 1 book chapter, numerous abstracts. The UIC faculty submitted 8 grant applications. Drs. Reed and Valenzuela were awarded an NIAID Clinical Trials in Organ Transplantation (CTOT) grant investigating the efficacy of Clazakizumab to improve long-term lung allograft and patient survival. Dr. Elaine Reed collaborating with Drs. Meghan Pearl and Patty Weng were awarded an NIH CTOT grant to advance renal transplantation outcomes in children. Dr. Reed received NIAID CIVIC grant option focused on immune profiling influenza vaccine responses and a Keck foundation grant to study immunity to SARS-CoV-2 in high risk health care workers. Dr. Reed received a philanthropic grant donation from an Aestiva Software Founder, to establish a post-doctoral research fellowship focused on understanding mechanisms of antibody mediated heart transplant rejection.
Reference
UIC has provided educational and proficiency testing programs to the Immunogenetics Community for 47 years. The UCLA Cell and DNA Exchange Programs manufactured 747 kits for 111 labs (49 Domestic/62 International labs) and analyzed and prepared the consensus report. The International HLA DNA Exchange program sent out 804 surveys to 134 laboratories (25 domestic/109 international). Given the recent interest in non-classical HLA genes in transplantation and disease association the UCLA Cell Exchange program added analysis and reporting of non-traditional HLA loci (HLA-E, -F, -G, -H, MICB) to the DNA Exchange proficiency test program.
UIC serves as CAP proficiency test provider since 2003 and manufactured kits for 900 clients across 8 surveys and received 100% grade for performance.
Innovation/Collaboration
In a cross-specialty collaboration, UIC took part in the development of the Tolerance Protocol in Renal Transplantation at UCLA. This groundbreaking science enables transplant recipients to thrive without immunosuppressive drugs. UCLA Health is one of the only five medical centers in the world capable of this approach in transplantation. The tolerance approach calls for blending the donor’s and recipient’s immune systems through an infusion of the organ donor’s stem cells shortly after the organ transplant. This blending method called, “Mixed Chimerism”, prompts the recipient’s body to recognize, rather than reject, the new organ. Since powerful medicines are filtered through the kidneys, a goal of the tolerance approach is to extend the survival of the transplanted kidney. While tolerance has been achieved in transplants with well-matched sibling donor-recipient pairs, UCLA Health physicians, in collaboration with OneLegacy, intend to expand the protocol to include deceased donors. This would allow for other kinds of transplants to be done without the necessity for lifelong immunosuppression-drug regimens.
We are grateful for institutional, quality, and research excellence on behalf of our UIC team. We look forward to their continued innovation!
April 2022
In addition to our Equity, Diversity, and Inclusion (EDI) Committee, our department also supports EDI within our research activities. I would like to spotlight our ongoing efforts to forward EDI in the research arenas.
Laboratory Medicine
- Omai Garner
- Title: PATHSUP: Precise Advanced Technologies and Health Systems for Underserved Populations.
- Description: Multi-institution, NSF-funded engineering project centered around creating cost-effective point of care devices for heart disease and diabetes, targeted at increasing access to historically underserved communities.
- Andrea McGonigle and Dr. Khalda Ibrahim
- Title: Leveraging Informatics Tools to Ensure High-Quality Transfusion Support for Patients with Sickle Cell Disease
- Description: Evaluating how implementation of informatics interventions can address the most significant information deficits (RBC genotype/phenotype, presence of alloantibodies and autoantibodies, history of transfusion and transfusion reactions) for providers and the blood bank, with the goal of improving care and health outcomes of patients with SCD.
- Lu Song
- Title: Impact of 2021 CKD-EPI equations
- Description: Evaluating the impact of the eGFR calculations using the 2021 CKD-EPI equations without race variables on the classifications of kidney impairment in our patient population.
UIC
- Elaine Reed
- Proposal under review by CEAL leaders Keith Norris and Arlene Brown entitled “Share, Trust, Organize, Partner: The COVID-19 California Alliance (STOP COVID-19 CA) Phase 3”
Subtitle: LA-SPARTA Synergy Operation COVID-19 (LASSO COVID-19)
Purpose: To advance mutual goals and synergistic opportunities for CEAL / STOP COVID-19 and LA-SPARTA with a focus on at-risk and underserved south LA populations disproportionately impacted by this pandemic. A translational purpose of this initiative is to enhance personal and public health education to promote improved outcomes in underserved persons at highest risks of exposure and greatest vaccine hesitancy.
- Identified differences in male vs female outcomes in our experimental outcomes of MRSA bacteremia. Our U19 application submitted last week focuses in part on defining host sex contexts that drive immune protection against exploitation by MRSA.
- Other funded research in ischemia reperfusion injury, immune signatures of CMV and Covid-19 infection that also include age, race, sex as predictors of outcome.
- Elaine F. Reed, in collaboration with the Women of FOCIS, has a manuscript with Frontiers Immunology under review.
- Elaine F. Reed, Anita Chong, Megan K. Levings, Caley Mutrie, Terri Laufer, Maria Grazia Roncarolo, Megan Sykes. The Women of FOCIS: promoting equality and inclusiveness in a professional federation of clinical immunology societies. Frontiers in Immunology, under review.
- Nicole Valenzuela
- As part of the Sensitization in Transplantation: Assessment of Risk (STAR) Consensus Workgroup on histocompatibility testing, we are highlighting the gap in representation of non-White HLA alleles on available commercial panels. We therefore are making recommendations to 1) expand the allele analytes to be more representation of diverse donor populations and 2) ensure rigor and accuracy in interpretation of non-White recipient testing for clinical diagnostics, investigative trials and research.
UIC + Anatomic Pathology
- Michelle Hickey (UIC) is working with anatomic pathologist Dr. Jonathan Zuckerman, informatics fellow Dr. Jitin Makker, and transplant nephrologist Dr. Eric Lum, to develop a data utility and visual analytics tool for transplant patient data. The utility will include clinical-diagnostic and health equity/disparity data to inform quality improvement and quality assurance.
- Rebecca Sosa, Bita Naini and Elaine Reed collaborated on a study to uncover underlying immune mechanisms of the well-known disparity experienced by Hispanic patients undergoing liver transplantation for nonalcoholic steatohepatitis (NASH). They investigated evolving patient immune status in comparison to clinical assays performed as part of standard of care. Hispanic liver transplant recipients with NASH were disproportionately female and disproportionately suffered poor outcomes in the first year post transplant, including rejection and death. Clinically, they saw increased AST/INR early post-transplant, increased histopathological features associated with NASH and IRI in post-reperfusion biopsies, and higher incidence of pre-sensitization to mismatched HLA antigens expressed by the donor allograft. Experimental investigation revealed an increase in leukocyte-attracting chemokines, innate-to-adaptive switching cytokines and growth factors, HMGB1 release and TLR4 activation. The study provides critical evidence that a more personalized approach towards reduction of risk factors is urgently needed for this immunological endotype in Hispanics with NASH requiring a liver transplant, particularly females.
Department
- Michelle Hickey, Director of Quality for UCLA Pathology and team organized the 2022 Quality Improvement Day and Daljit S. and Elaine Sarkaria Keynote Lecture which was held on February 11, 2022. The theme this year was stated as a question- “How can pathologists contribute to solving heath disparities and promote health equity?” We welcomed Dr. James Crawford Professor and Chair, Pathology and Laboratory Medicine, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell as well as three UCLA Faculty, Dr. Naveen Raja, Dr. Eric Cheng, and Dr. Susanne B Nicholas to present on topics of Value Based Care, Health Equity and Informatics. We also welcomed three trainees to discuss their quality improvement projects- Dr. Jitin Makker, Dr. Ali Samiei and Dr. Khalda Ibrahim.
As noted by leadership at our David Geffen School of Medicine, by educating the next generation of physicians, physician-scientists, and researchers, we will instill the core values of justice, equity, diversity, and inclusion that are inseparable from our institutional goals of excellence in all tenets of healthcare, research, education, and community engagement.
I am so proud of the EDI work being done by our faculty, our EDI committee and every member of our Department. We have done wonderful work this year, and I am excited to watch our efforts and accomplishments continue to grow!
March 2022
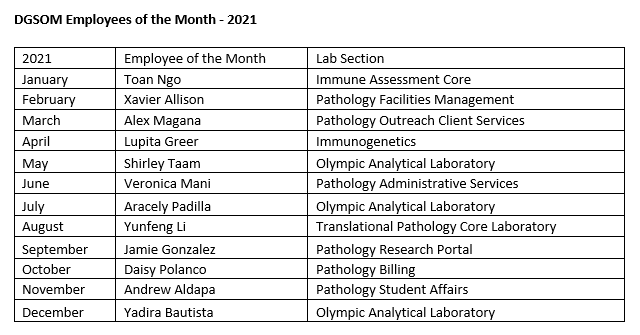
At the David Geffen School of Medicine, we believe that a strong organizational culture is critical to our ability to achieve our mission and vital to our well-being and cohesion as a community. The Cultural North Star helps us build and maintain an inclusive, mission-driven culture by mapping our decisions, actions and interactions to a shared framework. In that light, I would like to spotlight our monthly Staff Recognition Program. We thank these amazing individuals for their hard work, for their dedication to our patients, faculty and to their team, for the outstanding quality of their work and for their consistently helpful and positive outlook.

Blood & Platelet Center: Instituted a Virtual Recruitment Blood Drive involving local school districts during the pandemic when high school drives were not feasible. During the pandemic, the Blood & Platelet Center (BPC) built new connections in the community to support blood collections. The BPC recently partnered with five African American groups on campus to hold the first ever blood drive in honor of Black History Month. The BPC has implemented numerous AABB-recommended safety measures to protect donors and staff during the COVID-19 pandemic. Donations are essential to stabilize our inventory during the recent national blood shortage and can save lives!
Heart Walk: Nathan Okawa (RRUMC Core Lab) led the UCLA Heart Walk Challenge for the Department of Pathology and Laboratory Medicine. For the second year in a row, team Pathology & Lab Medicine raised the most money in the Health System, besting 43 other UCLA teams!
We look forward to finding innovative ways to support clinical care, our patients, and our community.
February 2022
Each day we strive to uphold the UCLA mission to heal humankind by delivering leading-edge research, education, patient care, and community engagement.
I am so proud of the many ways in which we have worked together to support our teams and to continue to offer the highest quality services possible to our patients during the recent Omicron surge. When our staff members, trainees and faculty were out sick with COVID, or taking care of sick family members, other staff members, managers, trainees, faculty and leadership stepped up to help out. These efforts ensured there was no disruption in any of our testing, including our COVID testing, which allowed our patients to receive the care they needed.
When our blood supplies became critically low, our Blood and Platelet Donor Center ramped up their efforts, collecting over 1200 units of O negative blood (as well as other whole blood and platelet donations) from December through mid-January. Our Transfusion Medicine faculty, fellows and residents tirelessly reviewed transfusion requests during the weeks of the most severe shortage to ensure blood products were used appropriately. This, combined with the immense help and support from our colleagues in Anesthesia and Surgery, helped us successfully manage a challenging situation. Thank you all!
Our Transfusion Medicine service and Blood and Platelet Center also participated in local and national collaborative projects to collect and provide COVID-19 Convalescent Plasma (CCP) during the pandemic. They collected 1,200+ CCP units from 250+ unique donors in 400+ visits, transfused approximately 20 patients as part of the Johns Hopkins CCP study, transfused 240+ UCLA patients as part of the Mayo study and shipped 500+ CCP to other hospitals as part of the Mayo study. We are so grateful to the leadership and vision of Dr. Alyssa Ziman, Transfusion Medicine Director, and all our Transfusion Medicine Faculty in agreeing to perform and collaborate on these studies, as well as to all our staff who helped collect, process and ship these units.
Our Clinical Microbiology lab performed over 175,000 COVID tests last calendar year. In comparison, the next highest volume test in the Microbiology area has 70,000 tests. Ramping up to perform this volume of tests would not have been possible without the dedication and support of our Microbiology staff, fellows and faculty, all of whom have gone above and beyond to ensure our patients and clinicians could get COVID tests when needed, and get their results within 1 day, and often within 8 hours. We are grateful to Dr. Omai Garner, Microbiology Section Chief, for his strategic thinking, creative problem solving and unfailingly positive attitude during the pandemic.
We were the only academic medical center in the LA area that had the facilities, such as a negative pressure room, required to perform autopsies on patients known or suspected to be positive for COVID. I am so grateful to Dr. Greg Fishbein, our Autopsy Service Chief, for his dedication and commitment to ensuring that families could obtain autopsies, and get important answers regarding their loved one, during COVID. Our Autopsy faculty, residents and staff handled a much higher volume of autopsies over the past two years with dedication, professionalism, and compassion, and in the process helped many families understand why their loved one had passed. These autopsies also helped the clinical providers better understand the pathophysiologic etiologies for their patients’ signs, symptoms and death.
Despite the changes we have endured due to COVID-19, hope and perseverance shine as brightly as our hard work and determination to serve the university, hospital, community, and beyond. I am proud of our accomplishments and that our Department provides so many essential contributions to UCLA Health and UCLA campus.
January 2022
At the David Geffen School of Medicine at UCLA (DGSOM), we believe that healthcare is a human right. We are educating the next generation of physicians, physician-scientists, and researchers with that belief in mind. The core values of justice, equity, diversity, and inclusion are inseparable from our institutional goals of excellence in all tenets of healthcare, research, education, and community engagement.
The Department of Pathology and Laboratory Medicine EDI Committee consists of over 50 members representing faculty, trainees, and staff from all areas of our Department, including Anatomic Pathology, Laboratory Medicine, Outreach, research, and education. The group is led by our co-chairs, Dr. Danny Rodriguez, Dr. Dawn Ward, Dr. David Lu, and Jennifer Filipek.

Our EDI Committee’s goals are to:
- Educate the department about unconscious bias, microaggressions, stereotypes, and other related topics
- Increase diversity in recruitments at the staff, trainee, and faculty levels
- Create a pipeline program in conjunction with DGSOM
- Increase diversity of speakers for departmental education and seminars
- Continuous review of diversity and equity data in the department to address any weaknesses that arise
The EDI Committee’s current focuses and subcommittees include:
- Residency Recruitment – The goal is to enhance diversity and equitable representation among trainee recruitment, address bias and privilege in the application process, and develop a sustainable systematic review process that holistically reviews applicants. This will be overseen by a subcommittee comprised of faculty, trainees, and education program staff. The subcommittee will review departmental data surrounding prior application cycles and recruitment, compile and aggregate data to identify valuable attributes that align with the department's mission, and develop a web-based holistic rubric to assess individual candidates.
- Book/Journal Club – Host discussion meetings on EDI related books/journals every three months, moderated by Dr. Steve Hart and Dr. Sarah Zhang. The first book selected is Caste by Isabel Wilkerson.
- Department Survey – The goal is to build a more diverse, equitable, and inclusive culture within the Department. Working with the DGSOM JEDI Office, we will develop a survey that will illustrate how employees, staff, and faculty experience our department’s culture and what is important to them. The survey’s output will generate qualitative data for the EDI committee to take action in creating a more inclusive, equitable, and diverse department.
- Pipeline Program – The goal is to work with DGSOM to implement pipeline with medical students, including activities for undergraduate, high school, and elementary school students. Another goal is to promote the pathology post-sophomore/junior fellowship (PSF/PJF) at regional and national events and identify a faculty lead for the PSF/PJF who will monitor the program goals, as well as provide mentorship. Additionally, the subcommittee will help facilitate local and virtual events to serve as a representative of Pathology and Laboratory Medicine and develop our EDI website in conjunction with the DGSOM to engage students.
- Grand Rounds – The goal is to ensure diversity of speakers and inclusion of EDI-related topics within the Grand Rounds series. The subcommittee’s role is to contribute ideas in terms of potential speakers and topics for the speaker series, collect data on speaker demographics and determine if there may be EDI deficiencies in the speaker lineup, and advise division leaders to consider speaker diversity for future presentations. We were delighted to host our first EDI Grand Rounds presentation on December 3, 2021, featuring Dr. Andrea Deyrup and Dr. Joseph Graves speaking on “Race in Medicine: Data or Distraction?”
For more information, please contact our EDI Co-Chairs at .