Meningioma Brain Tumor
Find your care
Our expert neurosurgery team is committed to providing the finest and most comprehensive patient care. For help finding a neurosurgeon, call .
What is a meningioma?
In this section: Definition | Symptoms | Diagnosis | Treatment | Prognosis

A meningioma is a tumor that arises from a layer of tissue (the meninges) that covers the brain and spine.
Meningiomas grow on the surface of the brain (or spinal cord), and therefore push the brain away rather than growing from within it. Most are considered “benign” because they are slow-growing with low potential to spread.
Meningioma tumors can become quite large. Diameters of 2 inches (5 cm.) are not uncommon. Meningiomas that grow quickly and exhibit cancer-like behavior are called atypical meningiomas or anaplastic meningiomas, and are fortunately rare.
Meningiomas represent about 20 percent of all tumors originating in the head and 10 percent of tumors of the spine.
About 6,500 people are diagnosed with meningiomas each year in the United States. This type of tumor occurs more frequently in people with a hereditary disorder called neurofibromatosis type 2 (NF-2).
from
on Vimeo.
The molecular genetics and tumor pathogenesis of meningiomas and the future directions of meningioma treatments.
Possible Symptoms Caused by a meningioma brain tumor
- The most common symptoms are pain (headache) for weeks to months, weakness or paralysis, visual field reduction and speech problems.
- Specific symptoms depend upon the location of the tumor. See the chart below:
Most Common Sites and Symptoms for Meningiomas in the Head:
Location - Convexity (on the surface of the brain away from the midline)
Common Symptoms - Seizures, headache, extremity weakness, difficulty speaking, visual field deficit.

Location - Parafalcine (arising the meningeal layer between the hemispheres of the brain)
Common Symptoms - Seizures, lower extremity weakness, headache, personality changes, dementia, increasing apathy, flattening of affect, unsteadiness, tremor.
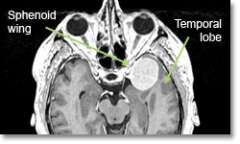
Location - Sphenoid Ridge
Common Symptoms - Eye-bulging, decreased vision, paralysis of eye movement, seizures, memory difficulty, personality change, headache.

Location - Posterior Fossa (area where the cerebellum is)
Common Symptoms - Unsteadiness and incoordination, hydrocephalus (increased pressure inside the brain), voice and swallowing difficulties.

Location - Cerebellopontine angle (on the side of the brainstem)
Common Symptoms - Loss of hearing. Facial muscle weakness. Dizziness. Unsteadiness and incoordination, hydrocephalus (increased pressure inside the brain), voice and swallowing difficulties.
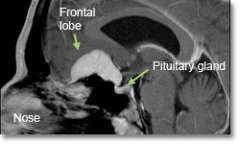
Location - Olfactory Groove and sella (bony space where the pituitary gland is situated)
Common Symptoms - Loss of smell (anosmia), subtle personality changes, mild difficulty with memory, euphoria, diminished concentration, urinary incontinence, visual impairment.
Optic Sheath - Decreased vision in one eye. | Other - Variable depending on location.
Diagnosis
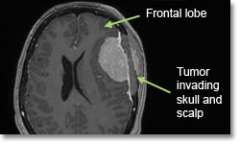
- Magnetic resonance imaging (MRI) scans effectively detect most meningiomas and are best at displaying details of the brain.
- Sometimes a CT scan is obtained to evaluate whether there is any bone (skull) involvement, or if the tumor is calcified.
Treatment
The decision of whether to, and how best to, treat a meningioma is based on multiple factors, including size and location of the tumor, symptoms, growth rate, and age of the patient (among others). In general, there are three basic options: observation, surgical removal, and radiation.
- Observation: Meningiomas are often slow growing, increasing is size only 1-2 mm per year. Repeating yearly MRI scans may be appropriate in the following situations:
- Patients with small tumors and mild or minimal symptoms, no impact on quality of life, and little or no swelling in adjacent brain areas.
- Older patients with very slowly progressing symptoms. Related seizures can be controlled with medication.
- Surgery: Meningioma surgery varies from relatively straightforward to highly complex, sometimes requiring multiple surgeons from different specialties.
- The ease of removal depends upon both their accessibility and the skill of the neurosurgeon. UCLA brain tumor neurosurgeons have extensive experience in removing all types of meningiomas.
- The goals of surgery are to:
- obtain tissue to confirm the diagnosis
- meningiomas are classified by pathologists into three types:
- Grade 1 - Benign: These very slow-growing tumors account for 75 percent of all meningiomas.
- Grade 2 - Atypical: Usually slow-growing but can recur.
- Grade 3 - Anaplastic: More malignant, faster-growing.
- The 15 percent of meningiomas that recur often progress to a higher grade. Grade 2 and 3 tumors recur more frequently than grade 1 types
- meningiomas are classified by pathologists into three types:
- remove sufficient tumor in order relieve pressure or distortion of the normal brain tissue
- When total removal of the tumor carries significant risk of morbidity (any side effect that can decrease quality of life), it’s better to leave some tumor tissue in place
- If the tumor invades any of the large draining veins, major arteries on the brain surface, or if it is on the underside of the brain, chances of a complete resection decrease and risk of complications increases.
- preserve and/or improve neurological function
- if possible and safe, remove all the tumor so that it will not grow back.
- Meningioma tumors that are near the surface and have not invaded deep structures or major blood vessels are more likely to be totally removed safely.
- obtain tissue to confirm the diagnosis
Minimally invasive surgical options available at UCLA

Endoscopic removal of meningiomas through the nose
- olfactory groove meningiomas
- tuberculum sella meningiomas
- sellar meningiomas

Keyhole microsurgical removal using eyebrow incision
- olfactory groove meningiomas
- sphenoid wing meningiomas

Endoport removal
- intraventricular meningiomas
- Tumor embolization prior to surgery
- In some cases, your surgeon may choose to reduce the blood supply to the tumor by ordering an embolization procedure.
- Embolization involves threading a thin tube (catheter) up the leg veins or arteries directly into the blood vessels that feed the tumor. Then a glue-like clotting substance is injected to choke off and shrink the tumor.
- Radiation
-
- For those ineligible for surgery or with incomplete surgical removal, either conventional radiation or fractionated stereotactic radiosurgery (radiotherapy) can slow or stop the growth of meningiomas.
- Radiation treatment is often considered for deep, surgically inaccessible tumors, or tumors in elderly patients.
- Younger patients (< 50 years of age) need to be counselled about the risk of developing radiation-induced cancer 10 or more years after radiation treatment. Fortunately, the chances of this happening appear to be very small.
- Meningiomas have sharp margins and rarely invade neighboring tissue, thus they are ideal tumors for focused, shaped radiation fields using the Novalis Shaped-Beam Surgery.

- This technique does not require actual surgery, but instead uses advanced imaging and computer technology to deliver a high dose of radiation to the tumor while limiting radiation exposure to the surrounding brain structures.
- For many meningioma tumors, the radiation field needs to be conformed to the shape of the tumor. In addition, delivering the radiation in smaller doses over a period of weeks will reduce the risk of injuring critical brain structures next to the tumor (which may cause blindness, deafness, paralysis). Some treatment techniques, such as the Gamma Knife, cannot deliver this type of treatment.
- UCLA neurosurgeons helped develop the Novalis Shaped-Beam Stereotactic System, one of the most advanced conformal stereotactic radiation delivery system in the world.
-
Prognosis
- Surgery
- For tumors in favorable locations, up to 85% of meningiomas are curable with surgery.
- Location, the amount of the tumor left after surgery, and the skill of the neurosurgeon are the important elements in predicting a successful result.
- Radiation
- Stereotactic radiosurgery stops the growth of meningiomas in up to 80 percent of cases.
The Neuro-ICU cares for patients with all types of neurosurgical and neurological injuries, including stroke, brain hemorrhage, trauma and tumors. We work in close cooperation with your surgeon or medical doctor with whom you have had initial contact. Together with the surgeon or medical doctor, the Neuro-ICU attending physician and team members direct your family member's care while in the ICU. The Neuro-ICU team consists of the bedside nurses, nurse practitioners, physicians in specialty training (Fellows) and attending physicians. UCLA Neuro ICU Family Guide