Metastatic Brain Tumors
Find your care
Our expert neurosurgery team is committed to providing the finest and most comprehensive patient care. For help finding a neurosurgeon, call .
About Metastatic Brain Tumors
- Metastatic brain tumors spread to the brain or spinal cord from cancer originating in other organs.
- Cerebral metastases are the most common type of “brain” tumor.
- Common brain metastases in adults come from the lung, breast, kidney, colon and skin (melanoma).
Diagnosis - Metastatic Brain Tumor
- Computed tomography (CT) or magnetic resonance imaging (MRI) scans are used to identify the tumors within the brain.
- Multiple tumors are found 35 percent to 50 percent of the time.
- In cases with no established diagnosis of cancer, a search for the primary site must be undertaken:
- Chest x-ray may visualize an obvious lung primary tumor or metastatic tumors to the lung.
- A CT scan of the chest and abdomen is a more sensitive study to look for small or deep tumors in the body.
- Mammogram in women.
- Whole body positron emission tomography (PET) scans can sometimes detect occult cancer.
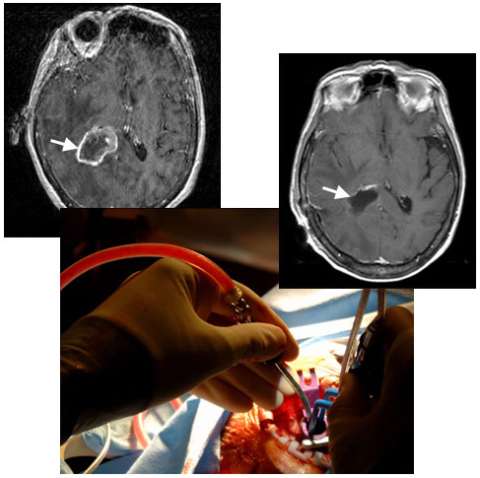
An MRI image (left) shows a metastatic brain tumor from lung cancer in the deep right parietal lobe (arrow). A photograph taken during surgery (center) shows the use a minimally-invasive port, only half an inch in diameter, to gain access so that the neurosurgeon can remove the tumor with minimal injury to the overlying normal brain. An MRI image following surgery (right) shows complete removal of the tumor (arrow) and the hardly visible surgical tract (below arrow).
Treatment - Metastatic Brain Tumor
The management of brain metastatic disease requires a multidisciplinary team approach, with input from the oncologist, radiation oncologist and neurosurgeon.
- Surgical management
- Surgery to remove single tumors may be indicated under the following circumstances:
- The primary disease is under control.
- The lesion is accessible and large in size.
- The lesion is symptomatic or life-threatening.
- The diagnosis is unknown.
- In some cases, such as failure to respond to other treatments, more than one metastatic tumor is considered for surgical removal.
- Micro-surgical techniques and state-of-the-art technology that minimize the trauma associated with surgical removal of metastases. UCLA neurosurgeons are experts in minimally invasive surgical techniques.
- UCLA neurosurgeons may recommend placing thin wafers containing chemotherapy (Gliadel wafers) into the surgical cavity to help kill residual microscopic cancer cells with a high concentration of chemotherapy only to that location. The procedure avoids intravenous chemotherapy.
- Stereotactic biopsy may be considered for deep lesions to establish the diagnosis.
- We use the complementary information obtained from multiple advanced brain mapping techniques, including positron emission tomography (PET) imaging, functional magnetic resonance imaging (fMRI) brain mapping and spectroscopic MRI imaging.
- When appropriate, the intra-operative MRI scanner may be used to provide intra-operative updated MR imaging to both guide the surgeon toward the tumor and to assess the results of tumor removal prior to completing surgery.
- Surgery to remove single tumors may be indicated under the following circumstances:
- Radiation therapy
- Stereotactic radiosurgery (SRS)
- SRS precisely delivers a high level of radiation to the tumor while giving the surrounding brain only small amounts of radiation exposure
- UCLA uses the Novalis shaped-beam system, which is equally or more effective as Gamma Knife.
- SRS can be used to treat up to seven small tumors (less than 2 cm in diameter).
- Regional brain radiation
- Radiation is delivered to a limited portion of the brain, typically reserved to the area surrounding a surgical resection
- Whole brain radiation
- Whole brain radiation is recommended for patients with multiple metastatic brain tumors if sole SRS is not an option.
- Although many radiation oncologists treat every patient with a brain metastasis with whole brain radiation, UCLA physicians use an individualistic approach and often recommend local radiation treatment only.
- Stereotactic radiosurgery (SRS)
- Medical management
- Anticonvulsants are sometimes prescribed to prevent seizures.
- Steroids may be necessary to decrease the amount of swelling.
- Chemotherapy may be offered by your oncologist.
The Neuro-ICU cares for patients with all types of neurosurgical and neurological injuries, including stroke, brain hemorrhage, trauma and tumors. We work in close cooperation with your surgeon or medical doctor with whom you have had initial contact. Together with the surgeon or medical doctor, the Neuro-ICU attending physician and team members direct your family member's care while in the ICU. The Neuro-ICU team consists of the bedside nurses, nurse practitioners, physicians in specialty training (Fellows) and attending physicians. UCLA Neuro ICU Family Guide