What is Alport syndrome?
Alport syndrome is a genetic, inherited disorder that runs in families.
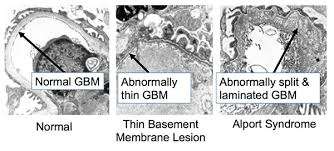
In a healthy kidney, nearly a million individual kidney subunits, called nephrons, filter blood through a spherical sac called the glomerulus. The glomerulus consists of a membrane, known as the glomerular basement membrane (GBM), that acts as a filtration barrier.
Healthy individuals also have a substance called collagen, of which there are several types, and in general all types provide structural support to various tissues. Type IV Collagen exists as a heterotrimer: three protein chains (α3, α3, and α3) intertwine.
In Alport syndrome, mutations in the genes COL4A3, COL4A4, and COL4A5, each responsible for coding their respective protein chains, cause a dysfunctional type IV collagen, which compromises the ability of the GBM to act as a filtration barrier. As a result, the GBM becomes leaky, and substances that should have been retained in the body are lost, including blood and proteins. The kidney tissue soon becomes permanently damaged and is replaced by fibrous tissue in a process called fibrosis. Finally, the kidney becomes so damaged that kidney failure may result, causing the patient to develop end stage renal disease, or ESRD.
It is important to note that Alport syndrome is a multisystem disease, as it also leads to hearing loss and ocular abnormalities.
How is Alport syndrome inherited?
Alport is a genetic disorder that can be passed down from parents in three different ways:
The first pattern of inheritance is called X-linked Alport syndrome (XLAS), in which the mutated gene is on the X-chromosome. Females have two copies of the X-chromosome, while males have a single copy, along with a Y-chromosome. Males typically show more severe symptoms, because females usually have an extra healthy X chromosome to mask the effect. 80% of all Alport cases are caused by this inheritance type. 50% of males require dialysis by age 25, and 90% develop ESRD by age 40.
The second pattern of inheritance is called autosomal recessive Alport syndrome (ARAS), in which the mutated gene is on a recessive autosome. 15% of all Alport cases are caused by this inheritance type. This disease has an early onset: kidney failure usually occurs by age 20.
The third pattern of inheritance is called autosomal dominant Alport syndrome (ADAS), in which the mutated gene is on a dominant autosome. 5% of all Alport cases are caused by this inheritance type. This disease has a delayed onset: ERSD typically occurs in middle age.



What are the incidence and prevalence of Alport syndrome?
Alport syndrome is the second most common cause of inherited kidney failure, after autosomal dominant polycystic kidney disease, or ADPKD.
The reported incidence is approximately 1 in 50,000 newborns. It affects roughly 30,000 to 60,000 people in the US currently. 3% of children diagnosed with chronic kidney disease (or CKD) and 0.2% of adults who have ERSD also have Alport syndrome. This lower percentage can perhaps be partially accounted for by the fact that many kids suffering from Alport syndrome do not make it to adulthood.
What are the symptoms of Alport syndrome?
- Hematuria, or blood in urine, since a faulty GBM causes blood to leak into the urine. Usually microscopic hematuria, in which the urine appears normal, but microscopic examination reveals red blood cells. Rarely, gross hematuria, which is distinguished by the appearance of bloody red urine.

Proteinuria, or protein in urine, since a faulty GBM causes proteins to leak into the urine. This is usually confirmed by albumin tests.
 Proteinuria
Proteinuria- Edema (swelling)
- Hypertension
- Ocular defects and sensorineural hearing loss
- Unfortunately, Alport syndrome is often quite asymptomatic until the very end. The best indicator of Alport syndrome, being a genetically inherited disease, is a family member with Alport syndrome.
How is Alport syndrome diagnosed?

People who suffer from Alport syndrome may have symptoms for years before being diagnosed: it is often asymptomatic until the very end, and having a family member with Alport syndrome is a key indicator of the need to be screened. Other methods of diagnosis include observation of the aforementioned clinical symptoms (hematuria, hearing loss, eye defects, swelling, proteinuria), lab tests (particularly for glomerular filtration rate, or GFR), genetic testing, skin and renal biopsies, and referral to ophthalmology and ENT (Ears, Nose, Throat) specialists for eye examinations and hearing tests.
Is there a treatment for Alport syndrome?
Alport syndrome cannot be specifically treated, as there are currently no specific and approved therapies for Alport syndrome. However, clinical trials are currently ongoing, so there may be an approved therapy in the near future.
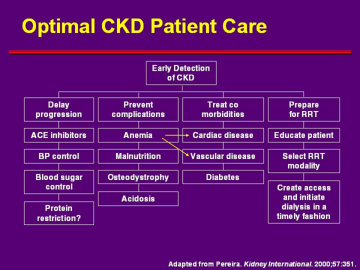
Moreover, since Alport syndrome is linked to CKD, measures can be taken to control CKD. These include ACEi (ACE inhibitors) and ARBs (Angiotensin II receptor blockers), which both help delay the progression of CKD. Just like Alport syndrome, CKD tends to be a silent disease, so early diagnosis is critical.
Excessive or deficient protein intake may put a patient at risk, requiring adequate control. Complications such as anemia, malnutrition, osteodystrophy, and acidosis should be closely monitored, as well as any risk from cardiac disease, vascular disease, and diabetes. Finally, the patient must play an active role in this whole process.

If a patient is in stage 5 CKD (kidney failure), dialysis or kidney transplants become a consideration. However, rarely, Alport Syndrome patients may suffer anti-GBM glomerulonephritis, a rare but dramatic complication that must be discussed with the transplant team.
Additionally, donors must also be screened carefully, particularly heterozygous females: there have been many cases of a carrier mother inadvertently transplanting her affected kidney to her son, which would be detrimental to both of them.
Note that the earlier the treatment, the better the outcomes!
Can Alport syndrome be prevented?
Alport syndrome is inherited, so it cannot be prevented. However, early diagnosis and an experienced, multidisciplinary medical team can provide the necessary care to slow down the progression of the disease and improve the quality of life in patients suffering from Alport syndrome. Patients are always advised to keep a detailed list of symptoms experienced and discuss it with their physician.
Alport Syndrome: What You Need to Know
Disclaimer: The UCLA Health System cannot guarantee the accuracy of such information. The information is provided without warranty or guarantee of any kind. Please speak to your Physician before making any changes.