Case: Axillary Lymphadenopathy
By Daniella Boros MD, and Manchandia Tejas MD
Introduction
Axillary lymphadenopathy can be caused by benign and malignant processes. In breast imaging, it important to distinguish normal lymph nodes from abnormal lymph nodes which often warrant additional workup.
Axillary Lymphadenopathy
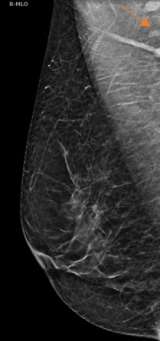
The axilla is partially imaging during mammography and axillary lymph nodes are commonly seen. Evaluation of lymph nodes on mammography involves assessment of laterality and lymph node morphology. Benign axillary lymph nodes (figure 1) are oval in shape, typically measuring less than 2 cm, with a preserved fatty hilum which appears as radiolucent notch on mammogram. Increased lymph node size or density can be abnormal, requiring additional evaluation1. In the case of abnormal lymphadenopathy, attention should be made to whether the lymph nodes are unilateral or bilateral as this can help narrow the differential diagnosis1,2.
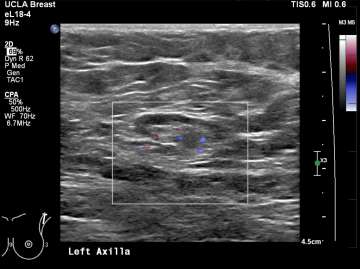
Ultrasound is the best modality for characterizing lymph nodes allowing for evaluation of shape, cortical thickness and presence or absence of fatty hilum. On ultrasound, normal axillary lymph nodes have an oval or lobulated shape with a preserved fatty hilum and cortical thickness less than 3 mm (figure 2). The echogenic hilum has arterial flow which can be assessed using color doppler imaging.
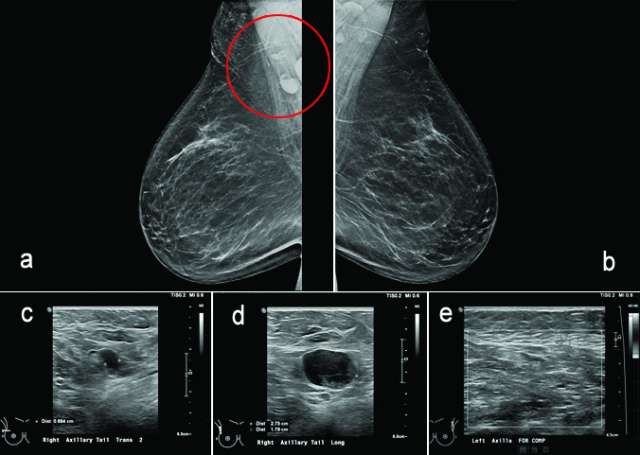
Features concerning for malignancy include round shape, increased cortical thickness and loss of fatty hilum1. The relationship of the lymph node cortex to hilum can be used to classify lymph node morphology and likelihood of malignancy. As the cortical thickness increases, there are reciprocal changes in the hilum beginning with hilar effacement and progressing to absence or replacement of the lymph node hilum2,3. Cortical thickening (figure 3) is considered the earliest morphologic change associated with malignancy; however, this finding is nonspecific with a low positive predictive value1-3. Absent/replaced hilum (figure 4) is the most specific for malignancy with a positive predictive value of 58-97%2.


The differential for abnormal axillary lymph nodes is divided into benign and malignant causes. Benign causes include reactive hyperplasia (i.e, skin or breast abscess, mastitis), autoimmune disease (i.e., rheumatoid arthritis, systemic lupus erythematous), HIV or granulomatous disease (tuberculosis, sarcoidosis). Lymphadenopathy associated with systemic processes is typically bilateral and symmetric1,2. Reactive lymphadenopathy can be unilateral/asymmetric in the setting of infection or recent vaccination3. Malignant cases of axillary lymphadenopathy include lymphoma/leukemia and metastatic disease. Bilateral and symmetric lymph node abnormalities are concerning for lymphoproliferative disorders such as leukemia/lymphoma. Unilateral lymphadenopathy raises suspicion for malignancy such as a primary breast cancer1,2,4.
Management of abnormal lymph nodes involves clinical correlation and additional evaluation. According to BIRADS, unilateral lymphadenopathy in the absence of infection/inflammatory causes is considered suspicious (BIRADS category 4). Evaluation of the ipsilateral breast should be performed to exclude a breast malignancy. Additionally, bilateral axillary ultrasound should be performed to confirm laterality. These findings should be correlated with clinical history and if lymphadenopathy is still unexplained, a biopsy should be performed. If a benign cause is identified, such as a skin lesion or breast abscess, a BIRADS category 2 (benign) is appropriate. Evaluation of bilateral lymphadenopathy follows a similar process. Bilateral axillary lymphadenopathy due to infectious/inflammatory conditions is assessed as a BIRADS category 2 (benign). In the case of malignant causes, BIRADS should be assigned according to the finding in the breast themselves. For example, if after review of clinical history, lymphadenopathy is determined to be due to known history of lymphoma, lymphadenopathy would be assessed as a category 2 (benign) as it relates to the breast. If lymphadenopathy is unexplained by clinical history, a biopsy should be performed (BIRADS category 4)4.
Case Examples
The following cases provide examples of axillary lymphadenopathy identified on screening mammography.
Figure 5, a-c.
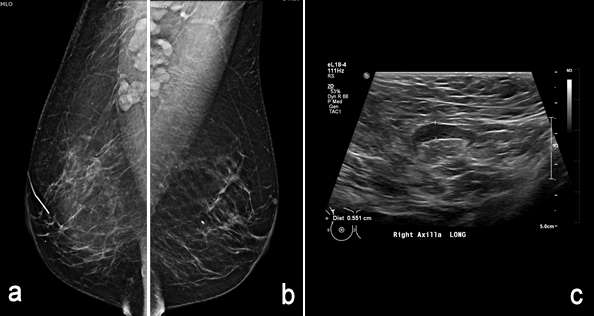
Figure 6, a-e.
Conclusion
Axillary lymphadenopathy is commonly encountered in breast imaging and can be associated with benign and malignant causes. Axillary lymph nodes are characterized according to morphology which includes cortical thickness and presence or absence of fatty hilum. Imaging characterization and clinical correlation is important to ensure appropriate diagnostic workup of axillary lymph nodes.
References
- Dialani V, James DF, Slanetz PJ. "A Practical Approach to Imaging the Axilla." Insights Imaging. 2015 Apr;6(2):217-29. . Epub 2014 Dec 23.PMID: 25534139
- Chung, H. L., Le-Petross, H. T., & Leung, J. W. (2021). "Imaging Updates to Breast Cancer Lymph Node Management." RadioGraphics, 2021 Sep-Oct;41(5):1283-1299. .
- Zhang, M., Ahn, R. W., Hayes, J. C., Seiler, S. J., Mootz, A. R., & Porembka, J. H. "Axillary lymphadenopathy in the COVID-19 ERA: What the Radiologist Needs to Know." RadioGraphics. 2022 Nov-Dec;42(7):1897-1911. . Epub 2022 Aug 26.PMID: 36018786
- D. Frequently Asked Questions - American College of Radiology. ACR BI-RADS® ATLAS — MAMMOGRAPHY. (n.d.). . Accessed 18 Aug 2023.