Case: Mastitis
by Zach Winchester, MD, Margit Szabari MD, Hannah Milch, MD
Mastitis is defined as inflammation of the breast with or without infection. It is a relatively common condition typically affecting reproductive age women. Mastitis can be sub-categorized into lactational (puerperal) mastitis and non-lactational (non-puerperal) mastitis.
Lactational mastitis
Lactational mastitis is usually caused by a combination of incomplete drainage of milk, focal engorgement of milk ducts, and introduction of bacteria through breaks in the overlying skin. Organisms are introduced into the ductal system, where they rapidly grow in stagnant milk and lead to infection of the milk ducts and surrounding breast tissue. It is typically seen within the first few weeks of breastfeeding, where bacteria from the infant’s mouth or mother’s skin enter through cracks or fissures in the nipple. Typical clinical findings include a focal, erythematous, painful area of one breast, with or without fever. Other symptoms may include chills, myalgias, and malaise. The most common causative organism is Staphylococcus aureus, followed by coagulase-negative staphylococci, while others include MRSA, Streptococcus pyogenes, Escherichia coli, and Bacteroides species. Some infections can be polymicrobial with a combination of aerobes and/or anaerobes. Risk factors include a history of mastitis, nipple cracks or fissures, maternal stress, inadequate drainage of milk, and tight-fitting bras.
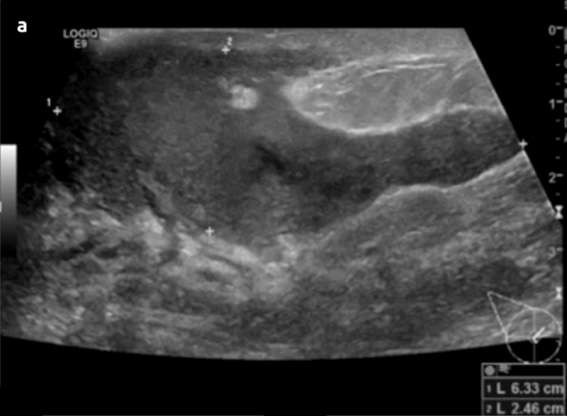
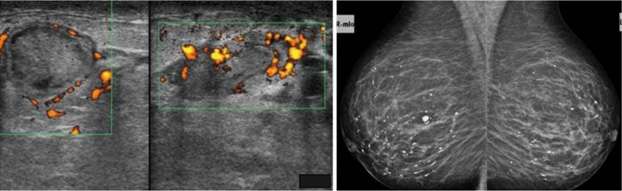
The most common complication includes breast abscess, occurring in 0.4-11% of patients with mastitis and is more frequently seen in cases of inadequately treated or late-presenting mastitis. If rupture of an abscess occurs, a resultant draining sinus and mammary fistula can occur. Diagnosis of lactational mastitis is based on clinical grounds, however ultrasound can be useful in differentiating between mastitis (ill-defined hypoechoic region) and a breast abscess (hypoechoic to anechoic mass with internal debris and surrounding vascularity) if there is a poor clinical response to antibiotics. Mammography is not usually performed but can show skin and trabecular thickening from breast edema.
Non-lactational Mastitis
Non-lactational mastitis is much less common than lactational mastitis and includes diagnoses such as periductal mastitis and idiopathic granulomatous mastitis.
Periductal mastitis is histopathologically defined as a chronic inflammatory condition of the major mammary ducts, with associated duct ectasia and plasma cell infiltration. It is usually seen in reproductive-age women. The cause and pathophysiology is not entirely understood. However, smoking appears to play a role in the development of this condition, either causing direct or indirect damage to the epithelial lining of the milk ducts, leading to inflammation, sloughing of epithelial cells, plugging and dilation of the duct and subsequent infection. Bacteria have also been implicated in the pathophysiology, with isolated organisms including Staphylococcus aureus, Enterococcus, Pseudomonas, Bacteroides, and Proteus species. Clinical symptoms include a subareolar mass with or without associated pain, erythema, nipple discharge, and/or nipple inversion. Imaging features on mammography include characteristic thick, linear, cigar-shaped or rod-like calcifications, with the long axis pointing toward the nipple. These calcifications tend to be longer, thicker, and smoother than calcifications seen with DCIS or ductal carcinoma. Sonographic features typically include dilated intramammary ducts with internal echogenic filling defects and increased surrounding vascularity. Complications are similar to lactational mastitis and include abscess and fistula formation.
Idiopathic granulomatous mastitis is another uncommon type of non-lactational mastitis that is usually seen a few years after lactation. The etiology and pathophysiology are also unclear but are currently thought to be related to an autoimmune process against specific antigens in extravasated milk. A reaction to breast trauma, subclinical infection (specifically with Corynebacterium species), and hyperprolactinemia have also been implicated in the etiology. It is thought that the resultant destruction of acini and milk ducts causes leakage of milk into breast tissue, triggering a localized inflammatory cellular infiltrate and ultimately a granulomatous response. Granulomatous mastitis usually presents as a unilateral firm breast mass, with or without skin thickening and ulceration, nipple retraction, and adenopathy. Often, patients present with extramammary symptoms including arthralgias and skin changes. Mammographic and sonographic appearance is variable. Mammograms are often normal but can also demonstrate asymmetrically increased density or multiple benign or malignant appearing masses. Ultrasound findings can include a mass-like appearance, tubular or nodular hypoechoic structures, or an ill-defined hypoechoic area. In the workup of this condition, other causes of granulomatous disease should be excluded, including sarcoidosis, granulomatosis with polyangiitis, tuberculosis, and fungal infection. Additionally, given similarity in presentation and imaging appearance, an underlying breast cancer should be excluded, and diagnosis is usually confirmed with biopsy of suspicious lesions. Complications also include abscess and fistula.

The initial treatment of lactational mastitis is symptomatic, with NSAIDs or acetaminophen for pain control, heat applied to the breast to facilitate milk drainage, and cold packs after emptying. Patients are encouraged to continue to breastfeed and/or pump throughout the process. Antibiotics are usually given if symptoms persist beyond 12 to 24 hours, usually with dicloxacillin or cephalexin as an outpatient to cover for S. aureus. If the patient has risk factors for MRSA, trimethoprim-sulfamethoxazole or clindamycin can be used. Periductal mastitis is empirically treated with amoxicillin-clavulanate, however it is often treated with surgical excision if recurrent. Lastly, there is no absolute consensus for treatment of granulomatous mastitis, with treatment strategies used including corticosteroids, antibiotics, immunosuppressants, and surgical excision. However, it often is self-resolving within a few months, and observation may be a sufficient treatment strategy in the appropriate setting. If a breast abscess is present, ultrasound-guided aspiration should be performed with cultures sent for sensitivities, and antibiotics should be initiated.
References
- Blackmon MM, Nguyen H, Mukherji P. "Acute Mastitis." [Updated 2022 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:
- Boakes E, Woods A, Johnson N, Kadoglou N. "Breast Infection: A Review of Diagnosis and Management Practices." Eur J Breast Health. 2018 Jul 1;14(3):136-143. PMID: 30123878; PMCID: PMC6092150.
- Dixon JM. "Periductal Mastitis/duct Ectasia." World J Surg. 1989 Nov-Dec;13(6):715-20. . PMID: 2696225.
- Leong PW, Chotai NC, Kulkarni S. "Imaging Features of Inflammatory Breast Disorders: A Pictorial Essay." Korean J Radiol. 2018 Jan-Feb;19(1):5-14. . Epub 2018 Jan 2. PMID: 29353994; PMCID: PMC5768507.
- Liu L, Zhou F, Wang P, Yu L, Ma Z, Li Y, Gao D, Zhang Q, Li L, Yu Z. "Periductal Mastitis: An Inflammatory Disease Related to Bacterial Infection and Consequent Immune Responses?" Mediators Inflamm. 2017;2017:5309081. . Epub 2017 Jan 15. PMID: 28182101; PMCID: PMC5274658.
- Memis A, Bilgen I, Ustun E, Ozdemir N, Erhan Y, Kapkac M. "Granulomatous Mastitis: Imaging Findings with Histopathologic Correlation." Clin Radiol. 2002 Nov;57(11):1001-6. .
- Omranipour R, Vasigh M. "Mastitis, Breast Abscess, and Granulomatous Mastitis." Adv Exp Med Biol. 2020;1252:53-61. . PMID: 32816262.
- Oztekin PS, Durhan G, Nercis Kosar P, Erel S, Hucumenoglu S. "Imaging Findings in Patients with Granulomatous Mastitis." Iran J Radiol. 2016 May 31;13(3):e33900. . PMID: 27853497; PMCID: PMC5107257.
- Sickles EA. "Breast Calcifications: Mammographic Evaluation." Radiology. 1986 Aug;160(2):289-93. . PMID: 3726103