Breast Ductal Anatomy and Function
By Arjun Ranade MD and Mollie Rashid MD
The breast is an intricate organ composed of adipose tissue and glandular tissue brought together by ligaments. Throughout the breast is a network of interconnecting ducts that carry milk from the lobules to the nipple. Familiarity with ductal anatomy is crucial for evaluating and understanding the different clinical and radiologic signs that may present with breast ductal abnormalities.
The breast ductal system starts as a network of smaller ducts within each mammary lobe and progressively merges to form larger ducts, ultimately leading to a single lactiferous duct. Multiple lactiferous ducts then drain into the nipple.
Key components of breast ductal anatomy include:
- Terminal Duct Lobular Unit (TDLU): The TDLU is the functional unit of the breast and consists of a lobule, its associated duct, and surrounding stromal tissue. The lobule is comprised of multiple acini, which are small glands surrounded by myoepithelial cells.
- Intralobular Ducts: Intralobular ducts arise from the acini within the lobules. These small ducts converge to form larger intralobular ducts, which connect to the interlobular ducts.
- Interlobular Ducts: Interlobular ducts are larger ducts that receive milk from the intralobular ducts. They traverse the stromal tissue and connect the multiple lobules within the breast. Interlobular ducts are lined by a layer of epithelial cells, supported by myoepithelial cells.
- Lactiferous Ducts: Lactiferous ducts are the final link within the ductal system. They are formed by the merging of multiple interlobular ducts and aid in the transport of milk from the TDLU to the nipple. Each breast typically contains 9 to 12 lactiferous ducts.
3 Essential Functions of the Breast Ductal System:
- Milk Production: The acini within the lobules primarily produce milk during lactation under the influence of hormones.
- Milk Transport: The interconnected network of intralobular and interlobular ducts allows the milk to be collected from multiple lobules and channeled into the lactiferous ducts, which converge at the nipple.
- Milk Ejection: Secondary to the coordinated contraction by myoepithelial cells surrounding the ductal systems, milk is driven forward until expression at the nipple.
Common Ductal Findings
- Duct ectasia
- Proteinaceous duct
- Solitary dilated duct
- Intraductal papilloma
Duct Ectasia
Breast duct ectasia, also sometimes known has plasma cell mastitis, is a benign condition characterized by the dilatation of multiple ducts. Although the exact etiology is unclear, it is likely secondary to chronic inflammation or fibrotic changes within the breast. It predominantly affects women older in age.
Clinical Signs of Duct Ectasia
- Nipple discharge is one of the hallmark clinical signs of duct ectasia. The discharge is usually non-bloody and can be thick, sticky, greenish, or brown in color. It may be intermittent and may originate from multiple duct openings.
- Many women with duct ectasia may experience breast pain and tenderness. The pain is typically localized around the nipple and may radiate to the surrounding breast tissue. The tenderness may be exacerbated by touch or pressure.
- Duct ectasia can cause structural changes in the breast resulting in a change of nipple appearance, such as nipple retraction or inversion. It is important to note that nipple retraction or inversion can also be a sign of other breast conditions, so further evaluation is usually necessary.
Radiology plays a crucial role in the evaluation and diagnosis of ductal ectasia, allowing for differentiation from other breast pathologies.
Mammographic features include:
- Sub-areolar linear or branching opacities which may be accompanied by rod-like calcifications.
- Due to the accumulation of fluid or inflammatory exudate within the dilated ducts, mammography may reveal round or oval shaped fluid-filled cysts. These cysts may demonstrate varying levels of opacity depending on the presence of intraductal debris.
- Of note, duct ectasia may not be fully seen on mammography.
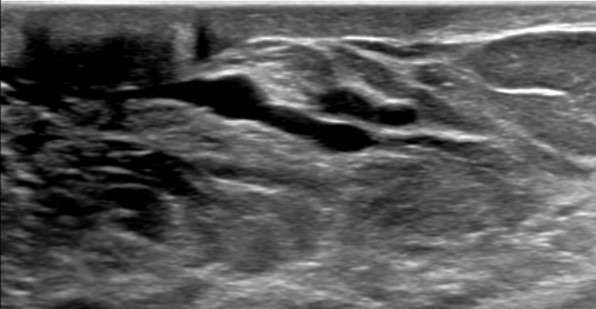
Ultrasound features include:
- Hypoechoic tubular structures measuring larger than 2 mm in diameter or 3 mm in diameter at the ampulla. These dilated ducts may be exhibit anechoic intraductal features secondary to simple fluid or low-level internal echoes secondary to intraductal debris.
- Inflammatory changes around the ducts, such as hypoechoic halo or echogenic strands, can be observed on ultrasound.
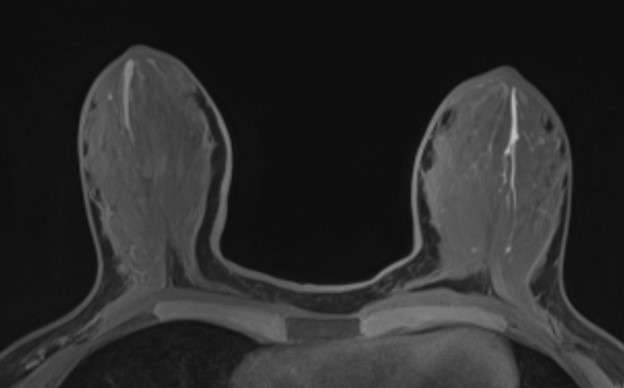
Magnetic Resonance Imaging (MRI) features include:
- Duct ectasia often presents as dilated tubular structures in a specific converging pattern towards the nipple, most often without contrast enhancement on MRI. They commonly exhibit T2 hyperintensity and T1 hypointensity.
- Inflammatory changes surrounding the dilated ducts can also be seen, presenting as increased signal intensity on T2-weighted images with or without enhancement on contrast enhanced images.
Proteinaceous Ducts
Proteinaceous ducts in the breast refer to the presence of abnormal accumulation of protein rich debris or fluid within the ductal system which may be secondary to chronic inflammation, infection, hormonal changes or obstruction. This can often present with ductal ectasia resulting in characteristic radiologic findings.
Mammographic features include:
- Findings may be similar to that of duct ectasia, as above.
Ultrasound features include:
- Proteinaceous fluid can often present with dilated ducts, which appear as hypoechoic tubular structures measuring 2 mm in diameter.
- The presence of proteinaceous material within the ducts may result in low level internal echoes and/or intraductal debris. This is often mobile or compressible.

MRI features include:
- Proteinaceous ducts may demonstrate ductal dilatation appearing as T2 hyperintense and sometimes T1 hyperintense tubular structures. Contrast enhancement is usually absent, indicating the presence of benign proteinaceous material.
Solitary Dilated Duct
A solitary dilated breast duct refers to the abnormal dilation of a single breast duct. It is a likely benign condition with low risk of malignancy that occurs most often secondary to chronic inflammation or fibrotic changes. However, asymmetric solitary dilated breast ducts in association with calcifications may trigger additional evaluation.
Mammographic features include:
- A solitary dilated breast duct can appear as a tubular radiopaque opacity demonstrating variable degrees of dilatation. There can be distortion of surrounding breast tissue.
- Coarse calcifications can be seen along the course of the dilated duct. These calcifications are typically benign and may result from chronic inflammation or stasis within the duct.
Ultrasound features include:
- A solitary dilated breast duct appears as a single tubular or cystic structure with variable echogenicity measuring 2 mm in diameter or 3 mm in diameter at the ampulla.
MRI features include:
- Solitary dilated duct typically appears as T2 hyperintense and T1 hypointense tubular structure. At times, T1 hyperintensity can be seen depending on the intraductal fluid content.
- Solitary dilated breast ducts typically demonstrate minimal to no enhancement, distinguishing them from more worrisome lesions.
Intraductal Papilloma
Intraductal papillomas are the most common benign ductal lesions that primarily affect women between ages of 40-50 years old. These benign lesions are often asymptomatic but can present with spontaneous nipple discharge or palpable lumps. Intraductal papillomas are commonly biopsied to exclude underlying atypia or neoplasia. Surgical consultation may be recommended to discuss management options, including watchful waiting and surgical excision.
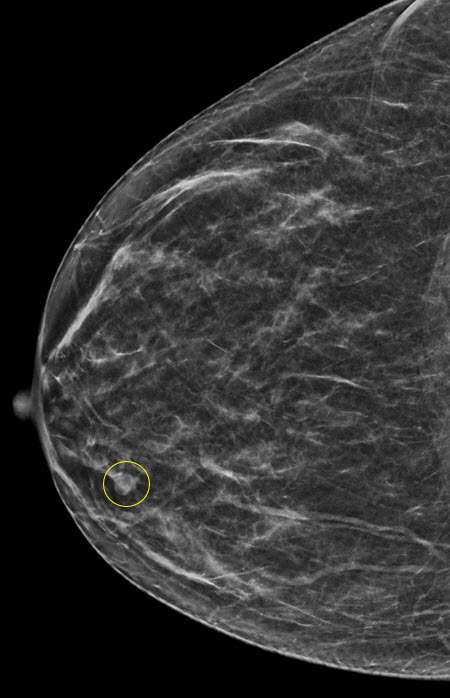
Mammographic features include:
- Intraductal papillomas may appear as well-circumscribed, round or oval opacities on often located in the subareolar region. Associated calcifications may be seen.
- In some cases, intraductal papillomas may present as only calcifications with varying morphology.
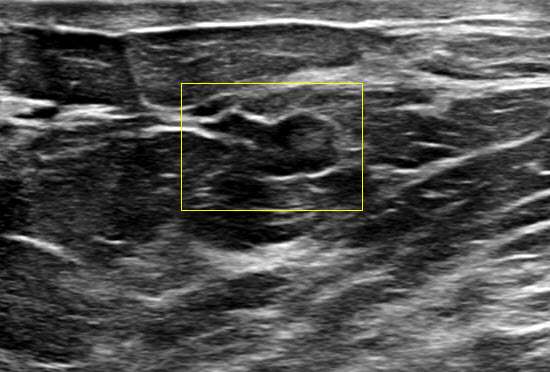
Ultrasound features include:
- Intraductal papillomas often appear as well defined solid intraductal masses within dilated ducts. They can exhibit a "frond-like" appearance projecting into the ductal lumen.
- Intraductal papillomas often demonstrate internal vascularity on color Doppler imaging. Furthermore, a vascular stalk may also be seen connecting to the ductal wall.
MRI features include:
- Intraductal papillomas can present as solid, circumscribed T2 hyperintense, T1 hypointense masses with smooth margins and associated ductal dilatation.
- They typically demonstrate contrast enhancement in a homogenous or heterogenous pattern.
References
- Zucca-Matthes G, Urban C, Vallejo A. "Anatomy of the Nipple and Breast Ducts." Gland Surg. 2016 Feb;5(1):32-6. . PMID: 26855906; PMCID: PMC4716863.
- Biswas SK, Banerjee S, Baker GW, Kuo CY, Chowdhury I. "The Mammary Gland: Basic Structure and Molecular Signaling during Development." Int J Mol Sci. 2022 Mar 31;23(7):3883. . PMID: 35409243; PMCID: PMC8998991.
- Choudhery S, Simmons C, Woodard GA, Bhatt AA, Anderson TL, Lee CU. "Outcomes of Solitary Dilated Breast Ducts in Symptomatic and Asymptomatic Patients." Br J Radiol. 2020 May 1;93(1109):20191039. . Epub 2020 Feb 28. PMID: 32101458; PMCID: PMC7217566.
- Li A, Kirk L. "Intraductal Papilloma." [Updated 2022 Sep 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from:
- "Duct Ectasia of the Breast: Mammary Duct Ectasia." Duct Ectasia of the Breast | Mammary.American Cancer Society. (n.d.).
- Hamwi, M Walid. “Mammary Duct Ectasia.” StatPearls [Internet]., U.S. National Library of Medicine, 17 July 2023, .
- Lee SJ, Sobel LD, Shamis M, Mahoney MC. "Asymmetric Ductal Ectasia: An Often Overlooked Sign of Malignancy." AJR Am J Roentgenol. 2019 Aug;213(2):473-481. . Epub 2019 Apr 17. PMID: 30995101.
- Ayres VJ, Ramalho LC, Wludarski SCL, Fleury EFC. "Screening a Solitary Dilated Duct in the Breast: A Pictorial Essay." Breast Cancer (Dove Med Press). 2021 Aug 12;13:505-512. . PMID: 34413680; PMCID: PMC8369045.
- Eiada R, Chong J, Kulkarni S, Goldberg F, Muradali D. "Papillary Lesions of the Breast: MRI, Ultrasound, and Mammographic Appearances." AJR Am J Roentgenol. 2012 Feb;198(2):264-71. . PMID: 22268167.